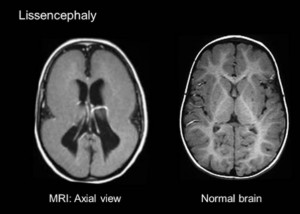
Lissencephaly, the literal meaning of which is ‘smooth brain’, is an uncommon, genetically-associated brain mal-development disorder marked by nil folds or convolutions in the cerebral cortex as well as microcephaly, i.e., an unusually small head. Lissencephaly is considered as a type of cephalic disorder. Terms like “pachygyria,” i.e., wide gyri or folds, or agyria, i.e., absence of gyri, are used by medical experts to define the appearance of brain surface in patients.
Sponsored link
Children affected by lissencephaly typically elicit considerable developmental delays, which in turn may vary from one affected child to another as per the severity of brain deformity and regulation of seizures. The life expectancy of the patients may be shortened, often because of underlying respiratory anomalies.
Lissencephaly is a very rare condition. In the US, it affects 11.7 children in every 1 million births.
Symptoms
Most children with lissencephaly tend to have a head which is of the normal size. However, some patients may be born with an abnormally small head, and the combination of the two brain-skull abnormalities is referred to as microlissencephaly.
Some of the additional common signs and symptoms of lissencephaly are listed below:
- Feeding difficulties
- Intellectual deficits
- Failure to flourish and thrive
- Irregular appearance of the face
- Swallowing problems
- Malformed toes, fingers, and/or hands.
- Severe psychomotor retardation
- Hypotonia or muscle spasms
- Seizures
Couples with a family history of lissencephaly can check for the presence of the condition via imaging tests. The brain normally develops folds during weeks 25 to 30 of pregnancy. This is when doctors will perform an ultrasound.
Lissencephaly Types
Advancements in the field of genetics and neuroimaging has facilitated better understanding of migration disorders, thereby allowing a better definition of the spectrum of lissencephaly. The spectrum is classified into nearly 20 different forms. Many more may be added after the respective causative factors have been discovered.
Lissencephaly is categorized as per varied systems. One of the major forms of classification is Classic/Type I vs. Cobblestone/Type II. However, certain systems and additional types cannot be added to any of these classifications.
A few types of lissencephaly are listed below, along with their OMM numbers:
1. Classic/Type I lissencephaly – 607432
- L1S1:This type of lissencephaly occurs due to mutation of PAFAH1B1 gene. It is further subdivided into:
- Miller–Dieker syndrome – 247200
- Type 1 isolated lissencephaly – 601545
- LISX1 – 300121:This type of lissencephaly occurs due to mutation of DCX/doublecortin gene. It is further subdivided into:
- Lissencephaly, isolated, type 1, without the occurrence of other known genetic errors.
2. Cobblestone/Type II lissencephaly
- Fukuyama syndrome – 253800
- Walker–Warburg syndrome, also known as HARD(E) syndrome – 236670
- MEB/Muscle-eye-brain disease – 253280
3. Other types of lissencephaly
Sponsored link
- Microlissencephaly, i.e., microcephaly and lissencephaly
- LIS3: TUBA1A – 611603
- LIS2: Norman-Roberts syndrome. It occurs due to RELN gene defects – 257320
- LISX2: ARX, 300215
Causes of lissencephaly
Lissencephaly is thought to be mainly caused due to certain genetic mutations. It can also occur due to inadequate blood flow to the brain of the unborn child during early pregnancy, or due to viral infections of the fetus or the uterus during the first trimester.
Any of the above listed factors can result in neural migration deficits at the time of embryo development. Neural migration is a process marked by movement of the nerve cells from their original place to the permanent area inside the gray matter of the cerebral cortex. Such migration or movement typically occurs between 12 and 14 weeks of fetal development. Lissencephaly develops because such movement of the nerve cells does not occur, eventually affecting the development of brain.
Studies have successfully found out that defects in the LIS1, DCX, 14-3-3ε, ARX, and RELN genes contribute towards the development of lissencephaly. The severity of the brain formation varies as per the type of gene that suffer from mutation.
Lissencephaly may occur on its own. It can also develop along with varied related conditions such as Walker-Warburg syndrome Miller-Dieker syndrome, isolated lissencephaly sequence, and Walker-Warburg syndrome. Specialists may be needed to differentiate between these varied disorders.
Couples at increased risk to conceiving a child with lissencephaly must go for genetic testing as well as genetic counselling before opting for parenthood.
Diagnosis
The brain surface of the fetus is usually smooth till week 25 to 30 of pregnancy. If routine complex ultrasound examinations performed after this period detect any cerebral abnormality, then doctors may recommend further testing such as NMR and genetic studies, especially if the unborn child has a family history of lissencephaly or other brain conditions, or if the doctor suspects the occurrence of brain defects. Chorionic villus sampling may also be performed to check the presence of certain variants of lissencephaly, if genetic mutations are detected.
After birth, if the baby shows signs and symptoms of brain malformation, then doctors may recommend varied diagnostic tests such as CT scans, MRI scans, and/or ultrasound. In case of lissencephaly, specialists will be needed to carefully grade the severity of brain malformation. A grade 1 lissencephaly diagnosis means that a large section of the brain is affected; it is extremely rare. Most lissencephaly patients suffer from grade 3 form of the disorder.
Treatment
Currently, there are no ways to medically correct the brain defects associated with lissencephaly. Treatment is dependent on the severity of the accompanying symptoms; it is aimed at managing the symptoms and preventing complications.
- Swallowing and feeding difficulties may need the use of a gastrostomy tube.
- Hydrocephalus is treated via shunting which helps remove excess cerebrospinal fluids.
- Seizures can be controlled with anticonvulsants and other anti-seizure medications.
Lissencephaly life expectancy
Life expectancy and prognosis of lissencephaly is dependent on the severity of the condition. The mental function in children with severe lissencephaly may not develop beyond that of a 3 to 5 months old baby. In the years gone by, such children did not live beyond 2 years. Now, the life expectancy has gone up to nearly ten years. Respiratory diseases, choking or aspiration on fluids or foods, and/or seizures are the main causes of death.
Child with mild instances of lissencephaly may feature near normal brain function and development.
Sponsored link



