Alpha 1 Antitrypsin Deficiency Alpha 1 antitrypsin is a type of protein produced in the liver and deficiency of this protein can cause liver problems and lung disease. A1AD is a genetic disorder inherited by birth. Any deficiency of this protein can damage the alveolar walls of the lungs. Normal serum level of A1A is about 20-60 umol/L and it can cause lung damage if the level goes below 15. Children having COPD (Chronic Obstructive Pulmonary Disease) should be checked for A1AT deficiency to prevent liver and lungs damage. A1AT is common disorder in white people and more particular in North western European countries.
A1AT is a under-diagnosed disorder and young children having frequent episodes of congestion may have this deficiency. About 10-15% of adults having A1AT disorder are likely to develop liver problems. There is no cure for A1AT but with early diagnosis symptoms can be managed and possible liver damage can be prevented. A1AT is also known as genetic emphysema, Alpha 1 emphysema and hereditary pulmonary emphysema.
Symptoms :
Initial signs of A1AT can appear even before 20 years. Some of the common symptoms include shortness of breath, wheezing, breathlessness while doing exercise, loss of weight, repeated respiratory infections, rapid heartbeat and extreme tiredness. The symptoms will increase steadily as the person smokes causing more damage to the lungs.
Some people may develop emphysema having symptoms of persistent cough, difficulty in breathing and barrel shaped chest. If the disease has progressed to cause liver damage the person may show symptoms like swollen legs or feet, swollen abdomen and yellow coloration of the skin.
Causes :
A1AT is an inherited disorder and the defective genes are passed on to the children. A genetic mutation in SERPINA1 gene is likely to cause A1AT disorder. This gene is responsible for producing antitrypsin protein which protects the body from neutrophil elastase. Actually elastase enzyme is meant for fighting infection, but if the level of A1AT is too low this enzyme can attack and destroy the lung walls called alveoli. This can lead to emphysema, a life threatening lung damage.
The defective gene of SERPINA1 is inherited by autosomal codominant method. People with two copies of M allele version will not develop A1AT deficiency. People having S allele version will have reduced production of antitrypsin enzyme and people with Z allele will have almost no enzyme secretion and they are prone to develop this disorder. Some people may have combination of version like SZ or SM or MZ and smoking considerably increases the risk of lung disorders. It is not true that every person with A1AT disorder would develop liver problem. Those having ZZ version are more likely to develop lungs and liver problems.
Tests :
Children with a history of A1AT disorder should be screened for serum levels frequently. The doctor will complete the physical exam and the symptoms. He would listen to the wheezing sound or shortness of breath using a stethoscope. He may order for blood test to identify Alpha 1 genotype, Alpha 1 antitrypsin test to find out the level of this protein serum in your blood. He may also order for imaging tests like chest X-ray to check how far the damage has been done. If he suspects liver problems he may conduct liver biopsy and liver function test.
Treatment :
A1AT disorder cannot be treated but the symptoms can be controlled. People with low levels of antitrypsin should be watched for symptoms. Such people will be advised to quit smoking to prevent early lung damage. Method of treatment varies with that of individual’s symptoms. Your doctor would prescribe suitable bronchodilators to control respiratory tract infection. People with COPD are given pulmonary rehabilitation. Such people can benefit by taking yearly shots of influenza vaccines. In severe cases lung surgery and transplantation is done. Liver problems can be managed by effective medications and specific diet. In extreme cases of liver failure, liver transplant is done.
Prognosis :
Those who are diagnosed with A1AT disorder in early stages (through screening tests before symptoms have developed) have better prognosis. Individuals diagnosed with COPD are likely to have Alpha 1 deficiency. A1AT is the top most risk factor causing emphysema. Hence everyone with COPD should be screened for Alpha 1.
All these diseases have early symptoms are expressed in a form that can recognize, find out the causes of the disease is the best way to get effective treatment and prevention best
Showing posts with label Prognosis. Show all posts
Showing posts with label Prognosis. Show all posts
Monday, March 30, 2015
Neurosarcoidosis
Neurosarcoidosis Sarcoidosis is described as a peculiar inflammatory disorder affecting the lungs and it occurs mostly between 20-40 years. It can affect many organs in the body since it is caused due to deposits of plaque like substance in the nervous system. Neuro-sarcoidosis is the term given to sarcoidosis that affects the nervous system. Often it affects the facial nerves and cranial nerves like pituitary gland and the hypothalamus.
People who have sarcoidosis have increased risk for developing neurosarcoidosis. Initial symptom of this disease is the Bell’s palsy causing weakness of optical (pertaining to eye) and auditory (ear) nerves. It can develop suddenly and also a slow process. Swelling of nerves can occur in any part of the body like brain or spinal cord or any other part of the nerves. The effects of this disease can be managed by taking corticosteroid drugs.
Causes :
Neurosarcoidosis is a chronic (long term) disorder affecting many organs and system of the body. It can affect particular area of nerves or the spinal cord as a whole. This disease develops due to the deposit of dead cells in the nerves thus disrupting its normal function.
Symptoms :
Muscle weakness in your face is the first symptom of neurosarcoidosis. The nerves of the face muscles can get affected causing intense pain or numbness in these areas. It can cause reduced vision, trouble in hearing and loss of smell and taste if the auditory and optical nerves gets affected. In case if the nervous system of the pituitary gland gets affected it can cause symptoms like excess of thirst, extreme tiredness, changes in menstrual cycle (for women) and increased urine output.
For some people it can cause symptoms like confusion, loss of memory, delirium, dizziness, blurred vision, headache, loss of taste or smell, seizures and stroke. If the peripheral nerves get affected due to this disorder, it can cause loss of sensation or abnormal sensation and reduced movement in particular part of the body.
Diagnosis :
Your doctor will complete physical exam after listening to your symptoms. He may then gather complete medical information and order for series of tests like blood profile, imaging tests like X-ray, CT or MRI scan of the brain. He may also perform lumbar puncture to collect cerebrospinal fluid inside and testing it in the lab. In case of inflammation of nerves the results would show increased levels of angiotensin converting enzyme.
Treatment :
Prognosis :
The outlook of this disease varies from one person to another. Age, health condition and intensity of nerves affected determine the prognosis. For some people the symptoms can be managed with effective doses of medications but for others the disease may progress repeatedly. For severe cases, it can cause permanent disability and even death. With progressive damage done to the brain nerves, there would be increased complications that can be serious.
Prevention :
You cannot totally prevent getting neurosarcoidosis. But if you are diagnosed with sarcoidosis, you need to get intense treatment for the disease so that it does not affect your nerves anymore.
People who have sarcoidosis have increased risk for developing neurosarcoidosis. Initial symptom of this disease is the Bell’s palsy causing weakness of optical (pertaining to eye) and auditory (ear) nerves. It can develop suddenly and also a slow process. Swelling of nerves can occur in any part of the body like brain or spinal cord or any other part of the nerves. The effects of this disease can be managed by taking corticosteroid drugs.
Causes :
Neurosarcoidosis is a chronic (long term) disorder affecting many organs and system of the body. It can affect particular area of nerves or the spinal cord as a whole. This disease develops due to the deposit of dead cells in the nerves thus disrupting its normal function.
Symptoms :
Muscle weakness in your face is the first symptom of neurosarcoidosis. The nerves of the face muscles can get affected causing intense pain or numbness in these areas. It can cause reduced vision, trouble in hearing and loss of smell and taste if the auditory and optical nerves gets affected. In case if the nervous system of the pituitary gland gets affected it can cause symptoms like excess of thirst, extreme tiredness, changes in menstrual cycle (for women) and increased urine output.
For some people it can cause symptoms like confusion, loss of memory, delirium, dizziness, blurred vision, headache, loss of taste or smell, seizures and stroke. If the peripheral nerves get affected due to this disorder, it can cause loss of sensation or abnormal sensation and reduced movement in particular part of the body.
Diagnosis :
Your doctor will complete physical exam after listening to your symptoms. He may then gather complete medical information and order for series of tests like blood profile, imaging tests like X-ray, CT or MRI scan of the brain. He may also perform lumbar puncture to collect cerebrospinal fluid inside and testing it in the lab. In case of inflammation of nerves the results would show increased levels of angiotensin converting enzyme.
Treatment :
- No clear treatment is available for neurosarcoidosis. The intensity of symptoms can be managed by effective drugs and therapies.
- Drugs that contain corticosteroid are prescribed for controlling swelling of nerves.
- Immunosuppressant drugs are also given for managing the symptoms.
- For people who have muscle weakness in particular part like hands or legs, physiotherapy is given for muscle relaxation.
- TNF alpha inhibitors are given to reduce inflammation of arthritis is effective in treating neurosarcoidosis.
Prognosis :
The outlook of this disease varies from one person to another. Age, health condition and intensity of nerves affected determine the prognosis. For some people the symptoms can be managed with effective doses of medications but for others the disease may progress repeatedly. For severe cases, it can cause permanent disability and even death. With progressive damage done to the brain nerves, there would be increased complications that can be serious.
Prevention :
You cannot totally prevent getting neurosarcoidosis. But if you are diagnosed with sarcoidosis, you need to get intense treatment for the disease so that it does not affect your nerves anymore.
Social Anxiety Disorder
Social Anxiety Disorder Social anxiety disorder is a problem that originates from the fear of making mistakes. The person with SA disorder will have unreasonable fear that he/she is being watched by others and will develop irrational fear of social situations. These people are always self conscious and worried about being criticized by others. People with SA disorder will often avoid being in social situations and if conditions compel them to take part in social events, they would develop an “anticipatory anxiety” probably weeks or even months before the occasion. They live in the fear of something wrong is going to happen. Many people are fully aware of their irrational fear (which is meaningless) but they don’t have the courage to overcome it.
SA disorder is called as “social phobia” which is linked with other type of mental issues like panic disorder or obsessive compulsive disorder. People with social phobia will have problems in interacting with people, and working in front of others. The fear becomes so intense that it seriously interferes with their routine activities and creates problems in relationships. These people are afraid to do even common things like using public toilet or eating in a restaurant etc. They imagine that somebody would criticize them for their behavior or mistakes and avoid such situations.
Causes :
No one factor can be limited to cause social anxiety disorder. It is caused by multiple factors like psychological, social and biological factors. For some people, SA disorder is hereditary and runs in families. It is believed to occur due to abnormal functions in the brain that is responsible for fear or stressful events.
For some people, SA disorder can develop due to embarrassing events in childhood and humiliating events in society during adolescence. Children with this disorder would have suffered and neglected by peers or bullied by others. Children who are over-protected may not have the opportunity to learn proper social skills and in later stage can develop this disorder.
Symptoms :
Some of the signs and symptoms of SA disorder are given below:-
Social anxiety disorder is ranked 2nd in general anxiety disorders and is ranked 3rd among various types of mental disorders. More than 15 million Americans are believed to have SA disorder. It begins during early childhood or adolescence mostly, but it can develop during adulthood also. More women develop SA disorder than men.
Diagnosis :
A person is said to have SA disorder if he/she has any of the above symptoms in the past 6 months. Parents can observe the behavior of their children in social situations and detect any such activities. Your doctor may conduct some physical tests to rule out any other physical problem. He may refer your child to psychiatrist who will evaluate SA disorder based on designed interview and various assessment tools.
Treatment :
Social Anxiety disorder can be fully treated and cured. But the rate of recovery will be fast if diagnosed in early stages. Your therapist would use a specialized method called cognitive behavior therapy for treating the symptoms. The person will be able to slowly overcome the fear and anxiety with regard to social events and situations. He would create artificial conditions resembling social setup and teach different ways of overcoming his fear. The therapist will also make your child learn social skills.
Medications are recommended to treat people with intense anxiety or depression associated with SA disorder. But you cannot expect results overnight and it may take several months or years to cope with anxiety prone situations. Social phobia can also be treated with monoamine oxidase inhibitor kind of drugs. These drugs can cause side effects and hence you have to visit your doctor regularly to report any changes.
Prognosis :
The outlook for SA disorder is satisfactory. Many people are able to live normal life and take part in social situations after therapy.
SA disorder is called as “social phobia” which is linked with other type of mental issues like panic disorder or obsessive compulsive disorder. People with social phobia will have problems in interacting with people, and working in front of others. The fear becomes so intense that it seriously interferes with their routine activities and creates problems in relationships. These people are afraid to do even common things like using public toilet or eating in a restaurant etc. They imagine that somebody would criticize them for their behavior or mistakes and avoid such situations.
Causes :
No one factor can be limited to cause social anxiety disorder. It is caused by multiple factors like psychological, social and biological factors. For some people, SA disorder is hereditary and runs in families. It is believed to occur due to abnormal functions in the brain that is responsible for fear or stressful events.
For some people, SA disorder can develop due to embarrassing events in childhood and humiliating events in society during adolescence. Children with this disorder would have suffered and neglected by peers or bullied by others. Children who are over-protected may not have the opportunity to learn proper social skills and in later stage can develop this disorder.
Symptoms :
Some of the signs and symptoms of SA disorder are given below:-
- Developing intense anxiety while taking part in social situations
- Feeling very self conscious in front of others
- Worried and anxious about particular event even days or weeks before
- Avoid taking part in social events
- Having unreasonable fear of getting criticized
- Having hard time to maintain friendship
- Developing physiological problems like trembling, sweating and blushing, shaking while attending social situations
Social anxiety disorder is ranked 2nd in general anxiety disorders and is ranked 3rd among various types of mental disorders. More than 15 million Americans are believed to have SA disorder. It begins during early childhood or adolescence mostly, but it can develop during adulthood also. More women develop SA disorder than men.
Diagnosis :
A person is said to have SA disorder if he/she has any of the above symptoms in the past 6 months. Parents can observe the behavior of their children in social situations and detect any such activities. Your doctor may conduct some physical tests to rule out any other physical problem. He may refer your child to psychiatrist who will evaluate SA disorder based on designed interview and various assessment tools.
Treatment :
Social Anxiety disorder can be fully treated and cured. But the rate of recovery will be fast if diagnosed in early stages. Your therapist would use a specialized method called cognitive behavior therapy for treating the symptoms. The person will be able to slowly overcome the fear and anxiety with regard to social events and situations. He would create artificial conditions resembling social setup and teach different ways of overcoming his fear. The therapist will also make your child learn social skills.
Medications are recommended to treat people with intense anxiety or depression associated with SA disorder. But you cannot expect results overnight and it may take several months or years to cope with anxiety prone situations. Social phobia can also be treated with monoamine oxidase inhibitor kind of drugs. These drugs can cause side effects and hence you have to visit your doctor regularly to report any changes.
Prognosis :
The outlook for SA disorder is satisfactory. Many people are able to live normal life and take part in social situations after therapy.
Post Traumatic Stress Disorder
Post Traumatic Stress Disorder Post traumatic stress disorder was earlier known as “shell shock” is a serious mental condition that occurs to a person who undergoes or witness a traumatic event. People who experience terrifying event in their life would take some time to overgrow the trauma. But for few people, the symptoms of helplessness, intense fear, flashbacks, nightmares, negative feelings and avoiding social life would continue for years after the event.
Actual cause of PTSD is not known clearly, since not all the people who witness traumatic events in their life are developing this disorder. It is believed to occur due to certain changes in chemical reaction in the brain. The symptoms can be managed with effective medications and therapy. Report indicates that 3.5-4% of Americans have PTSD (about 7.8 million Americans). This disorder can occur to anyone at any age and more women than men suffer from this anxiety disorder.
Symptoms :
Initial symptoms would start anytime after a person experiences traumatic event. The signs and symptoms can be broadly categorized into 4 main streams namely disturbed memories, avoidance, having negative changes in mood and finally change in emotions. Disturbed memories can cause recurrent thoughts about traumatic event, flashbacks, nightmares, upsetting dreams and intense emotional disturbance.
Symptoms of avoidance include avoiding people, avoiding certain places and avoiding thinking or talking about the stressful event. Negative changes in mood and thought can cause guilt feeling, low self esteem, hopelessness, lack of interest and inability to maintain relationships. The person may not remember certain aspects of the event and he may lose interest in important activities.
Changes in emotions can cause difficulty in sleeping, concentrating, guilt feeling, and trouble in remembering and concentrating, always expecting some danger and engaging in self destructive behavior. The person may get frightened easily even by small events. The intensity of symptoms may not be the same for all. The memories would become severe when the person is stressed or witness certain events that remind them about the past. Children with PTSD at young ages can have delayed development of motor skills.
Causes :
PTSD is classified as an anxiety disorder affecting certain people who witness terrifying event or undergo increased stress. A child who is sexually abused for prolonged period may develop PTSD. An individual who witness gruesome accident, who is in part of personal assault, who sees violent deaths of loved ones and military combat can develop this disorder.
People who are held as captives by terrorists and those who are part of natural disasters can have high risk of developing traumatic disorder. Symptoms can begin shortly within weeks but for some people it might take months or years also. PTSD is believed to occur due to inherited mental aspects of your personality and the response of your body to stressful events and changes in chemical reaction in your brain.
Who are at Risk?
Diagnosis :
PTSD can be detected based on symptoms. Your doctor will refer the case to a psychologist who will evaluate the disorder by asking series of questions. She would ask you about the traumatic events in your life. According to the Diagnostic and Statistical Manual of psychiatric disorders, a person is said to have PTSD if he/she has some of the above mentioned symptoms for more than a month or two. For some people it can cause great distress and make them unable to carry on with daily tasks.
Treatment :
The main purpose of treating PTSD is to help the person to overcome the stress caused by traumatic event or experience. Based on the severity of the symptoms, the person will be given psychotherapy and medications.
Cognitive behavior therapy can help the person to change his thought patterns and manage his feelings and emotions caused by trauma. Exposure therapy is one in which the therapist will take the person through artificially created traumatic experience and teach him to confront the fear. Many approaches like psychodynamic therapy, family and group therapy are used to change the behavior of the person effectively and to remove the distress caused by traumatic experience.
Antidepressants like sertraline or paroxetine are prescribed for relieving symptoms of anxiety and depression. Anti anxiety drugs can help the person to overcome stress and improve his sleeping pattern. Prazosin is an effective drug used to control nightmares and relieve the symptoms of PTSD. You need to consult your doctor about the side effects of these medications and follow his instructions and usage and dose.
Discuss with your doctor and therapist freely about PTSD. Stick on to your treatment plan even if you feel better and continue taking medications till your doctor says to stop them. Do regular exercise and eat healthy diet. Get in touch with your family and friends and share your feelings. You can also join a support group to get ideas about their coping strategies.
Many of us would confront with traumatic experience in life, but not all of us develop symptoms of PTSD. You will be able to come out of it within few days. Do not delay in getting treatment if you feel that you are not able to overcome the stress caused by traumatic experience. The more you delay the treatment, the more will be the severity of symptoms of PTSD.
Prognosis :
In most of the cases, recovery is possible but it can take some time since it is a gradual process. You cannot totally forget the event but you can manage to carry on with life with well developed coping methods.
Actual cause of PTSD is not known clearly, since not all the people who witness traumatic events in their life are developing this disorder. It is believed to occur due to certain changes in chemical reaction in the brain. The symptoms can be managed with effective medications and therapy. Report indicates that 3.5-4% of Americans have PTSD (about 7.8 million Americans). This disorder can occur to anyone at any age and more women than men suffer from this anxiety disorder.
Symptoms :
Initial symptoms would start anytime after a person experiences traumatic event. The signs and symptoms can be broadly categorized into 4 main streams namely disturbed memories, avoidance, having negative changes in mood and finally change in emotions. Disturbed memories can cause recurrent thoughts about traumatic event, flashbacks, nightmares, upsetting dreams and intense emotional disturbance.
Symptoms of avoidance include avoiding people, avoiding certain places and avoiding thinking or talking about the stressful event. Negative changes in mood and thought can cause guilt feeling, low self esteem, hopelessness, lack of interest and inability to maintain relationships. The person may not remember certain aspects of the event and he may lose interest in important activities.
Changes in emotions can cause difficulty in sleeping, concentrating, guilt feeling, and trouble in remembering and concentrating, always expecting some danger and engaging in self destructive behavior. The person may get frightened easily even by small events. The intensity of symptoms may not be the same for all. The memories would become severe when the person is stressed or witness certain events that remind them about the past. Children with PTSD at young ages can have delayed development of motor skills.
Causes :
PTSD is classified as an anxiety disorder affecting certain people who witness terrifying event or undergo increased stress. A child who is sexually abused for prolonged period may develop PTSD. An individual who witness gruesome accident, who is in part of personal assault, who sees violent deaths of loved ones and military combat can develop this disorder.
People who are held as captives by terrorists and those who are part of natural disasters can have high risk of developing traumatic disorder. Symptoms can begin shortly within weeks but for some people it might take months or years also. PTSD is believed to occur due to inherited mental aspects of your personality and the response of your body to stressful events and changes in chemical reaction in your brain.
Who are at Risk?
- Military personnel and people facing prolonged physical or mental abuse are at high risk of developing PTSD.
- People who lack good family system and grow up in neglected childhood have increased chance of getting this disorder.
- You are at risk of getting this problem if you have family history of anxiety disorder or other mental health problem.
- People who are involved in natural disasters like flood, earthquake and who witness’s accident or plane crash may develop PTSD.
- As such PTSD can cause complications like depression, anxiety and emotional disturbance if not treated. It can cause complications like developing addiction to alcohol or substance and increased suicidal thoughts.
Diagnosis :
PTSD can be detected based on symptoms. Your doctor will refer the case to a psychologist who will evaluate the disorder by asking series of questions. She would ask you about the traumatic events in your life. According to the Diagnostic and Statistical Manual of psychiatric disorders, a person is said to have PTSD if he/she has some of the above mentioned symptoms for more than a month or two. For some people it can cause great distress and make them unable to carry on with daily tasks.
Treatment :
The main purpose of treating PTSD is to help the person to overcome the stress caused by traumatic event or experience. Based on the severity of the symptoms, the person will be given psychotherapy and medications.
- Psychotherapy :
Cognitive behavior therapy can help the person to change his thought patterns and manage his feelings and emotions caused by trauma. Exposure therapy is one in which the therapist will take the person through artificially created traumatic experience and teach him to confront the fear. Many approaches like psychodynamic therapy, family and group therapy are used to change the behavior of the person effectively and to remove the distress caused by traumatic experience.
- Medications :
Antidepressants like sertraline or paroxetine are prescribed for relieving symptoms of anxiety and depression. Anti anxiety drugs can help the person to overcome stress and improve his sleeping pattern. Prazosin is an effective drug used to control nightmares and relieve the symptoms of PTSD. You need to consult your doctor about the side effects of these medications and follow his instructions and usage and dose.
Discuss with your doctor and therapist freely about PTSD. Stick on to your treatment plan even if you feel better and continue taking medications till your doctor says to stop them. Do regular exercise and eat healthy diet. Get in touch with your family and friends and share your feelings. You can also join a support group to get ideas about their coping strategies.
Many of us would confront with traumatic experience in life, but not all of us develop symptoms of PTSD. You will be able to come out of it within few days. Do not delay in getting treatment if you feel that you are not able to overcome the stress caused by traumatic experience. The more you delay the treatment, the more will be the severity of symptoms of PTSD.
Prognosis :
In most of the cases, recovery is possible but it can take some time since it is a gradual process. You cannot totally forget the event but you can manage to carry on with life with well developed coping methods.
Tuesday, April 1, 2014
Paranoid Personality Disorder
Paranoid Personality Disorder Paranoid personality disorder is characterized by odd/eccentric thinking. The affected people have paranoia with insistent mistrust on others. They would always doubt on others even though there is no reason for it. This disorder manifests in early adulthood and is found more in men than women. The personality of any person is shaped according to the way in which he/she perceives and relates the world. Some types of personality disorders show peculiar behavior that deviates clearly from the social norms. Any person is said to have personality disorder only if his behavior or thinking is different, rigid and inflexible and causes significant impairment in relationships with others.
People with paranoid personality disorder have a tendency to interpret other people action as deliberately threatening. They will always have feelings of distrust, unknown fear and unjustified suspicion on others. These people are seen often misinterpreting other’s comments/behavior that induces them to develop baseless resentment for them for long time.
Symptoms :
The intense doubts of these people would interfere with the ability to make close relationships. Some of the signs of paranoid personality disorder are:-
Causes :
Like many other personality disorders the exact cause for PPD is not known. It can be due to multiple factors including hereditary, biological as well as environmental factors. Individuals with close relative having schizophrenia or other mental illness are prone to develop PPD and other types of personality problems. Negative childhood experiences and neglect or baseless parental rage can cause this problem.
Diagnoses :
The doctor will collect complete history of the affected child/person from parents and close relatives. He would also gather information about the mental health of his relatives. He would then refer the case to any psychologist or psychiatrist who will use the tools like questionnaire or other assessment methods for studying the nature of personality.
Treatment :
Individuals with paranoid personality will not accept that they have a problem. It is the duty of loved ones or close relatives to encourage them to take treatment with psychologist. Psychotherapy is often used for improving coping skills of the concerned person which in turn would increase his self esteem and communication skills. Since these people will not trust others, they will find some reason to skip the therapy sessions. It can be challenging for the therapist to convince them initially. It is really difficult to make them to stick on the treatment plan. But without treatment this disorder can become worse spoiling their relationships at office. It can lead to loss of employment or disruption of relationship with spouses.
The therapist will devise comprehensive plan for includes family support for reducing the symptoms. They would also require consistent therapy depending on the intensity of their symptoms and poor adjustments. Many times these people will terminate the therapy sessions finding some faults or excuses. Building client-therapist rapport is difficult with paranoid people. Medications are rarely given to these people only if they have depression/anxiety disorder. If the symptoms are severe anti-psychotic drugs are prescribed for relaxation.
Prognosis :
In case the disorder is chronic the person will need lifetime treatment. There are people who are able to manage relationships and jobs with paranoid personality. But many others will have tough time to maintain their relations/jobs making life complicated. The outcome may be poor if there is no continuity in the treatment plan.
People with paranoid personality disorder have a tendency to interpret other people action as deliberately threatening. They will always have feelings of distrust, unknown fear and unjustified suspicion on others. These people are seen often misinterpreting other’s comments/behavior that induces them to develop baseless resentment for them for long time.
Symptoms :
The intense doubts of these people would interfere with the ability to make close relationships. Some of the signs of paranoid personality disorder are:-
- Doubt the loyalty of others all the time. Having intense suspicion that each person around them are deceiving them
- Will not reveal any personal information to others due to fear that others will misuse against them
- Hold grudges on others and will not accept criticism
- Perceive casual looks as purposeful and will identify some hidden meanings in any remarks
- Have suspicion on others without any reason and will react violently and fast in responding
- Cannot maintain good relationships even with spouse or lovers
- Cannot accept their role in any problem since according to them they are always right
- Very stubborn, argumentative and socially isolate
Causes :
Like many other personality disorders the exact cause for PPD is not known. It can be due to multiple factors including hereditary, biological as well as environmental factors. Individuals with close relative having schizophrenia or other mental illness are prone to develop PPD and other types of personality problems. Negative childhood experiences and neglect or baseless parental rage can cause this problem.
Diagnoses :
The doctor will collect complete history of the affected child/person from parents and close relatives. He would also gather information about the mental health of his relatives. He would then refer the case to any psychologist or psychiatrist who will use the tools like questionnaire or other assessment methods for studying the nature of personality.
Treatment :
Individuals with paranoid personality will not accept that they have a problem. It is the duty of loved ones or close relatives to encourage them to take treatment with psychologist. Psychotherapy is often used for improving coping skills of the concerned person which in turn would increase his self esteem and communication skills. Since these people will not trust others, they will find some reason to skip the therapy sessions. It can be challenging for the therapist to convince them initially. It is really difficult to make them to stick on the treatment plan. But without treatment this disorder can become worse spoiling their relationships at office. It can lead to loss of employment or disruption of relationship with spouses.
The therapist will devise comprehensive plan for includes family support for reducing the symptoms. They would also require consistent therapy depending on the intensity of their symptoms and poor adjustments. Many times these people will terminate the therapy sessions finding some faults or excuses. Building client-therapist rapport is difficult with paranoid people. Medications are rarely given to these people only if they have depression/anxiety disorder. If the symptoms are severe anti-psychotic drugs are prescribed for relaxation.
Prognosis :
In case the disorder is chronic the person will need lifetime treatment. There are people who are able to manage relationships and jobs with paranoid personality. But many others will have tough time to maintain their relations/jobs making life complicated. The outcome may be poor if there is no continuity in the treatment plan.
Monday, March 17, 2014
Pneumothorax
Pneumothorax Pneumothorax is a condition that collapses the lung due to accumulation of air in the thoracic cavity. Spontaneously pneumothorax can occur without any underlying disease or condition. Sometimes it develops as a process due to underlying disease. Slowly, the air leaks into the gap available between the lungs and chest wall exerting force on the lungs making it to collapse. Even injury or strong blow to the lungs (during surgical procedures) can cause pneumothorax. This condition can be treated by aspiration or removal of free air collected in the chest cavity. In some cases the entire lungs collapses due to pneumothorax and in other cases only a portion of the lung collapses.
Symptoms :
Sudden chest pain is the first symptom of pneumothorax. Unlike other chest pain which worsens during inhaling air this type of chest pain stays on the same position and intensity. As the lung collapses either partially or fully it causes shortness of breath either in mild form or severely. If there is breathing difficulty and sudden chest pain you should visit the nearest hospital without delay. Prompt treatment is necessary when a person suffers from breathing problem with chest pain. It can be indicative of other problems also.
Causes :
Lung collapse or pneumothorax can occur due to sudden chest injury or due to lung infection or disease. In some cases, pneumothorax may develop without any obvious reason. Chest injury can be the outcome of gunshot, car accident, sudden blow, and fracture in the ribs, cardiopulmonary resuscitation, lung biopsy and certain medical procedures.
Underlying lung infection like pneumonia, tuberculosis, emphysema, lung cancer, cystic fibrosis and pulmonary fibrosis can cause pneumothorax. Sometimes, minute quantities of air blisters (called blebs) may develop on the top of lungs. Apparently there is no cause why only certain people develop these blebs. Certain procedures of flying or scuba diving may lead to the formation of blebs. People who are put on artificial respiration methods like ventilator have chance for developing pneumothorax. It can also develop due to prolonged asthma, COPD and lung cancer.
Who are at risk?
Men are at increased risk for developing pneumothorax when compared with women. Individuals of age group 20-40 years and those who are very thin and tall are prone to develop this problem. Having lung disease like pulmonary fibrosis or cystic fibrosis and prolonged use of ventilator machine for breathing can also develop pneumothorax. Genetics play a role for causing this disease. People with family history of pneumothorax are prone to this sudden lung collapse.
Complications :
Pneumothorax if unattended can lead to cardiac arrest and respiratory failure. In severe cases it can cause death.
Tests :
Chest X-ray of the affected person can show exact picture of lung collapse. Sometimes your doctor may request for imaging tests like CT for getting detailed image of the disease.
Treatment :
The aim of the treatment is to relieve the pressure caused by air leakage from the lungs. The method of treatment depends on the severity of pneumothorax and how far the lung has collapsed causing damage. Observation and monitoring is enough for individuals who have small portion of lung collapse. Your doctor will monitor the health condition by chest X-rays and watch whether the air is getting absorbed completely and if the lung has expanded fully to the normal position. If required, your doctor may give supplemental oxygen for speeding up the process.
Chest tube insertion is the process in which hollow tube is inserted into the ribs of the lung cage to remove the air. Through the needle a syringe is attached on the other end so that the doctor can blow out the excess of air. For some people, chest tubes are attached for several days to the patient so that suction device can be used to pump out the excess air.
Surgery :
Surgery is done for closing the air leakage in the lungs. It can be done by making small incision through special long handled tools. The surgeon will look for blebs inside and sew it properly. He would also apply talk like material in the space so that it prevents leakage of air in future.
Pictures of Pneumothorax :
Images, Pics, Pictures and Photos of Pneumothorax



Prognosis :
Most of the cases of pneumothorax surgery will resolve. Small air leakage will not require any surgery and can be managed by other methods like chest tube insertion. In case if the problem arises due to long term lung infections then it carries risk. Further such type of pneumothorax requires immediate medical attention. In many cases pneumothorax (lung collapse) may recur again (about 40%). Hence once you are diagnosed with pneumothorax it is necessary to monitor your health condition continuously.
Symptoms :
Sudden chest pain is the first symptom of pneumothorax. Unlike other chest pain which worsens during inhaling air this type of chest pain stays on the same position and intensity. As the lung collapses either partially or fully it causes shortness of breath either in mild form or severely. If there is breathing difficulty and sudden chest pain you should visit the nearest hospital without delay. Prompt treatment is necessary when a person suffers from breathing problem with chest pain. It can be indicative of other problems also.
Causes :
Lung collapse or pneumothorax can occur due to sudden chest injury or due to lung infection or disease. In some cases, pneumothorax may develop without any obvious reason. Chest injury can be the outcome of gunshot, car accident, sudden blow, and fracture in the ribs, cardiopulmonary resuscitation, lung biopsy and certain medical procedures.
Underlying lung infection like pneumonia, tuberculosis, emphysema, lung cancer, cystic fibrosis and pulmonary fibrosis can cause pneumothorax. Sometimes, minute quantities of air blisters (called blebs) may develop on the top of lungs. Apparently there is no cause why only certain people develop these blebs. Certain procedures of flying or scuba diving may lead to the formation of blebs. People who are put on artificial respiration methods like ventilator have chance for developing pneumothorax. It can also develop due to prolonged asthma, COPD and lung cancer.
Who are at risk?
Men are at increased risk for developing pneumothorax when compared with women. Individuals of age group 20-40 years and those who are very thin and tall are prone to develop this problem. Having lung disease like pulmonary fibrosis or cystic fibrosis and prolonged use of ventilator machine for breathing can also develop pneumothorax. Genetics play a role for causing this disease. People with family history of pneumothorax are prone to this sudden lung collapse.
Complications :
Pneumothorax if unattended can lead to cardiac arrest and respiratory failure. In severe cases it can cause death.
Tests :
Chest X-ray of the affected person can show exact picture of lung collapse. Sometimes your doctor may request for imaging tests like CT for getting detailed image of the disease.
Treatment :
The aim of the treatment is to relieve the pressure caused by air leakage from the lungs. The method of treatment depends on the severity of pneumothorax and how far the lung has collapsed causing damage. Observation and monitoring is enough for individuals who have small portion of lung collapse. Your doctor will monitor the health condition by chest X-rays and watch whether the air is getting absorbed completely and if the lung has expanded fully to the normal position. If required, your doctor may give supplemental oxygen for speeding up the process.
Chest tube insertion is the process in which hollow tube is inserted into the ribs of the lung cage to remove the air. Through the needle a syringe is attached on the other end so that the doctor can blow out the excess of air. For some people, chest tubes are attached for several days to the patient so that suction device can be used to pump out the excess air.
Surgery :
Surgery is done for closing the air leakage in the lungs. It can be done by making small incision through special long handled tools. The surgeon will look for blebs inside and sew it properly. He would also apply talk like material in the space so that it prevents leakage of air in future.
Pictures of Pneumothorax :
Images, Pics, Pictures and Photos of Pneumothorax



Prognosis :
Most of the cases of pneumothorax surgery will resolve. Small air leakage will not require any surgery and can be managed by other methods like chest tube insertion. In case if the problem arises due to long term lung infections then it carries risk. Further such type of pneumothorax requires immediate medical attention. In many cases pneumothorax (lung collapse) may recur again (about 40%). Hence once you are diagnosed with pneumothorax it is necessary to monitor your health condition continuously.
Labels:
Causes,
Complications,
define pneumothorax,
Diseasespictures,
Pictures of Pneumothorax,
pneumothorax causes,
pneumothorax symptoms,
pneumothorax treatment,
Prognosis,
spontaneous pneumothorax,
Surgery,
Symptomspneumothorax,
tension pneumothorax,
Tests,
Treatment,
what is pneumothorax,
Who are at risk
Sunday, October 13, 2013
Prader-Willi Syndrome – Symptoms, Diagnosis, Treatment, Prognosis, Life Expectancy, Pictures
Prader-Willi Syndrome – Symptoms, Diagnosis, Treatment, Prognosis, Life Expectancy, Pictures
This is an uncommon condition which is existent at birth and can result in numerous mental, behavioral as well as physical problems. A major component of Prader-Willi syndrome is the endless feeling of hunger that normally starts after the age of one.
Individuals with this syndrome constantly need to eat and normally have problems monitoring their weight. Many of the difficulties of Prader-Willi syndrome are because of obesity.
If the child has Prader-Willie syndrome, a specialists team will work with the parents to manage the symptoms the child has as well as reduce any risk of the development of complications.
The symptoms and signs normally happened in 2 stages. Signs and symptoms of this disorder that may be present in the 1st year of life consist of:
Muscle tone that is poor
This is a major sign of this syndrome during infancy – hypotonia. Infants may rest with knees as well as elbows extended loosely rather than fixed and this give the feeling of being floppy or like rag dolls when being held.
Facial features
Those with this syndrome can be born with eyes that are almond-shaped, turned down mouth, narrowing of the head at the temples as well as an upper lip that is thin All facial features which are distinct.
Eye coordination is lacking – Strabismus
The eyes of a child with this syndrome may not interchange together. They can wander to the side or be crossed.
Failure to thrive
Children with this syndrome during the first year can have a sucking reflex that is poor due to muscle tone being decreased. Since poor sucking makes feeding problematic, there will be a trend for slow weight gain.
Overall poor responsiveness
The baby might seem very tired, respond badly to stimulation, have difficulty waking as well as have a cry that is weak.
From the age of one to four, other signs or symptoms will appear. These difficulties will stay present thru out life and careful treatment or management is required. These signs or symptoms may include:
Weight gain and food cravings
The classic signs of this disorder will appear – food craving and rapid gaining of weight. The child with this syndrome is always hungry, consumes large portions of food and eats frequently. They may also be unusual food seeking behaviors such as eating or hoarding food such as frozen food or garbage.
Sex organs that are underdeveloped
A condition known as hypogonadism will occur resulting in underdeveloped organs, incomplete development at puberty as well as infertility in almost all cases. Females may not start periods until 30s or may never have them. Males may not have any facial hair and the voice might not fully deepen.
Poor physical development and growth
Those with Prader-Willi syndrome have very low muscle mass. They also have short feet and hands. When they reach full adult stature, they are normally shorter than other members of the family.
Learning problems
Moderate or mild cognitive impairment is a feature that is common for those with this disorder. Basically all individuals with this syndrome, even without substantial cognitive in capacity, will have disabilities with learning.
Motor development delayed
Toddlers with this syndrome usually reach milestones in movement physically later than other children. For instance, sitting up without help can be late as much as twelve months as well as not walking until 2 years.
Problems with speech
Speech can be delayed until the child is two years old or older. Articulation of words often is an ongoing disability.
Problems with behavior
Children can be very stubborn and throw temper tantrums, particularly when it comes to food being denied. Other mental health problems can develop such as picking at skin.
Disorders sleeping
Some with this syndrome can have problems with sleep, including normal sleep cycle interruptions as well as sleep apnea. Obesity will only worsen sleep disorders.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
Scoliosis
Numerous children with this syndrome develop an abnormal curvature of the spine or scoliosis.
Other symptoms and signs of Prader-Willi syndrome can include:
It is important to get an accurate and prompt diagnosis. You should see your physician if your infant:
With older children see the physician if the child shows any of the below signs:
In infants, the signs and symptoms that might cause your physician to order a blood test for Prader-Willi syndrome can include:
With children who are older, the physician might suspect this syndrome if the child shows:
A definitive diagnosis may always be made with a lab test. Genetic testing can detect anomalies in the child’s chromosomes that are specific for Prader-Willi syndrome.
A health professional team will work with the parents in order to help in the management of the child’s disorder. The majority of children with the syndrome will require the below treatments as well as care:
Infant nutrition
Most infants with this syndrome have problems with feeding because of muscle tone that is decreased. The child’s physician might advise a formula that is high-calorie in order for the infant to gain weight as well as monitoring the child’s development.
Treatment with growth hormone
This stimulates growth as well as influences the body’s exchange of diet into energy or metabolism. Studies have shown that growth hormonal treatment with this syndrome aids in increasing growth, decreases body fat, improves muscle tone – but the effects long-term of growth hormonal treatment are not known. An endocrinologist can aid in determining if the child will receive help from growth hormonal treatment.
Treatment with sex hormone
The endocrinologist might suggest that the child also take “hormone replacement therapy” which involves testosterone therapy for males or progesterone as well as estrogen for females. This can help in decreasing the child’s risk of osteoporosis.
Diet
As the child ages, a nutritionist can help develop a reduced-calorie, healthy diet in order to keep the child’s weight controlled as well as confirming appropriate nutrition.
Development overall
The child can benefit from a wide range of management therapies, including speech therapy, physical therapy as well as occupational therapy. Developmental therapy also helps in learning behaviors that are appropriate for their age, interpersonal skills as well as social skills.
Mental health
A professional in mental health can help with any psychological problems that the child might have for instance mood disorder, obsessive-compulsive. Some children will benefit from medication to manage behavioral problems.
Adult care transition
Most individuals with this syndrome will need supervision and specialized care thru out their lives. Most adults may live in a residential care facility that helps them with eating healthy diets, work, living safely and enjoying leisure events.
When obesity is evaded and difficulties are managed well, life expectancy for individuals with this syndrome is normal or very near normal. Most individuals will lead lives that are healthy if diagnosis is early and a management or treatment plan is in place to avoid any complications especially with obesity that is uncontrolled.
As previous stated with early diagnosis and management of complications, life expectancy for individuals with Prader-Willi syndrome is normal or near normal. But there is some literature that suggests a life expectancy of not past the age of 40.



What is Prader-Willi Syndrome?
This is an uncommon condition which is existent at birth and can result in numerous mental, behavioral as well as physical problems. A major component of Prader-Willi syndrome is the endless feeling of hunger that normally starts after the age of one.
Individuals with this syndrome constantly need to eat and normally have problems monitoring their weight. Many of the difficulties of Prader-Willi syndrome are because of obesity.
If the child has Prader-Willie syndrome, a specialists team will work with the parents to manage the symptoms the child has as well as reduce any risk of the development of complications.
Prader-Willi Syndrome Symptoms
The symptoms and signs normally happened in 2 stages. Signs and symptoms of this disorder that may be present in the 1st year of life consist of:
Muscle tone that is poor
This is a major sign of this syndrome during infancy – hypotonia. Infants may rest with knees as well as elbows extended loosely rather than fixed and this give the feeling of being floppy or like rag dolls when being held.
Facial features
Those with this syndrome can be born with eyes that are almond-shaped, turned down mouth, narrowing of the head at the temples as well as an upper lip that is thin All facial features which are distinct.
Eye coordination is lacking – Strabismus
The eyes of a child with this syndrome may not interchange together. They can wander to the side or be crossed.
Failure to thrive
Children with this syndrome during the first year can have a sucking reflex that is poor due to muscle tone being decreased. Since poor sucking makes feeding problematic, there will be a trend for slow weight gain.
Overall poor responsiveness
The baby might seem very tired, respond badly to stimulation, have difficulty waking as well as have a cry that is weak.
From the age of one to four, other signs or symptoms will appear. These difficulties will stay present thru out life and careful treatment or management is required. These signs or symptoms may include:
Weight gain and food cravings
The classic signs of this disorder will appear – food craving and rapid gaining of weight. The child with this syndrome is always hungry, consumes large portions of food and eats frequently. They may also be unusual food seeking behaviors such as eating or hoarding food such as frozen food or garbage.
Sex organs that are underdeveloped
A condition known as hypogonadism will occur resulting in underdeveloped organs, incomplete development at puberty as well as infertility in almost all cases. Females may not start periods until 30s or may never have them. Males may not have any facial hair and the voice might not fully deepen.
Poor physical development and growth
Those with Prader-Willi syndrome have very low muscle mass. They also have short feet and hands. When they reach full adult stature, they are normally shorter than other members of the family.
Learning problems
Moderate or mild cognitive impairment is a feature that is common for those with this disorder. Basically all individuals with this syndrome, even without substantial cognitive in capacity, will have disabilities with learning.
Motor development delayed
Toddlers with this syndrome usually reach milestones in movement physically later than other children. For instance, sitting up without help can be late as much as twelve months as well as not walking until 2 years.
Problems with speech
Speech can be delayed until the child is two years old or older. Articulation of words often is an ongoing disability.
Problems with behavior
Children can be very stubborn and throw temper tantrums, particularly when it comes to food being denied. Other mental health problems can develop such as picking at skin.
Disorders sleeping
Some with this syndrome can have problems with sleep, including normal sleep cycle interruptions as well as sleep apnea. Obesity will only worsen sleep disorders.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
Scoliosis
Numerous children with this syndrome develop an abnormal curvature of the spine or scoliosis.
Other symptoms and signs of Prader-Willi syndrome can include:
- Light skin as compared with other members of the family
- Nearsightedness or myopia
- Pain tolerance that is high
It is important to get an accurate and prompt diagnosis. You should see your physician if your infant:
- Has problems feeding
- Does not respond to touch
- Does not wake easily
- Has rag doll like limbs
With older children see the physician if the child shows any of the below signs:
- Weight gain that is rapid
- Unusual food-seeking behaviors
- Constant hunger
Prader-Willi Syndrome Diagnosis
In infants, the signs and symptoms that might cause your physician to order a blood test for Prader-Willi syndrome can include:
- Muscle tone that is poor
- Eyes that are almond shaped
- Head narrowing at the temples
With children who are older, the physician might suspect this syndrome if the child shows:
- Weight gain
- Behavioral problems
A definitive diagnosis may always be made with a lab test. Genetic testing can detect anomalies in the child’s chromosomes that are specific for Prader-Willi syndrome.
Prader-Willi Syndrome Treatment
A health professional team will work with the parents in order to help in the management of the child’s disorder. The majority of children with the syndrome will require the below treatments as well as care:
Infant nutrition
Most infants with this syndrome have problems with feeding because of muscle tone that is decreased. The child’s physician might advise a formula that is high-calorie in order for the infant to gain weight as well as monitoring the child’s development.
Treatment with growth hormone
This stimulates growth as well as influences the body’s exchange of diet into energy or metabolism. Studies have shown that growth hormonal treatment with this syndrome aids in increasing growth, decreases body fat, improves muscle tone – but the effects long-term of growth hormonal treatment are not known. An endocrinologist can aid in determining if the child will receive help from growth hormonal treatment.
Treatment with sex hormone
The endocrinologist might suggest that the child also take “hormone replacement therapy” which involves testosterone therapy for males or progesterone as well as estrogen for females. This can help in decreasing the child’s risk of osteoporosis.
Diet
As the child ages, a nutritionist can help develop a reduced-calorie, healthy diet in order to keep the child’s weight controlled as well as confirming appropriate nutrition.
Development overall
The child can benefit from a wide range of management therapies, including speech therapy, physical therapy as well as occupational therapy. Developmental therapy also helps in learning behaviors that are appropriate for their age, interpersonal skills as well as social skills.
Mental health
A professional in mental health can help with any psychological problems that the child might have for instance mood disorder, obsessive-compulsive. Some children will benefit from medication to manage behavioral problems.
Adult care transition
Most individuals with this syndrome will need supervision and specialized care thru out their lives. Most adults may live in a residential care facility that helps them with eating healthy diets, work, living safely and enjoying leisure events.
Prognosis
When obesity is evaded and difficulties are managed well, life expectancy for individuals with this syndrome is normal or very near normal. Most individuals will lead lives that are healthy if diagnosis is early and a management or treatment plan is in place to avoid any complications especially with obesity that is uncontrolled.
Prader-Willi Syndrome Life Expectancy
As previous stated with early diagnosis and management of complications, life expectancy for individuals with Prader-Willi syndrome is normal or near normal. But there is some literature that suggests a life expectancy of not past the age of 40.
Prader-Willi Syndrome Pictures



Noonan Syndrome – Symptoms, Treatment, Prognosis, Life Expectancy, Pictures
Noonan Syndrome – Symptoms, Treatment, Prognosis, Life Expectancy, Pictures
This is a disorder that is caused by a mutation that is genetic and stops the usual development in varied areas of the body. This syndrome can affect an individual in varied way such as:
This syndrome occurs when the fetus receives a copy of the gene that is affected from one parent. This is known as “dominant inheritance”. It may occur also as a mutation that is spontaneous, which means that there is no history of this disorder in the family.
There is currently no precise treatment for this syndrome. Treatment is focused on managing the disorder’s symptoms as well as difficulties that can arise. Growth hormone can be needed to manage short stature in certain individuals with this syndrome.
Facial features
The way an individual’s face appears is one of the main clues which leads to the diagnosis of this syndrome. These appearances or signs alter with age:
Early infancy
When the baby is younger than one month old, it can have eyes that are down-slanting and wide set, ears that are low-set, groove that is deep and peaks that are wide in the upper lip, neck that is short as well as a hairline that is low in the back.
Infancy
The baby can have eyes that are prominent that slant downward as well as lids that are thickened and a nose depressed at the top with a base that is wide and a tip that is bulbous.
Childhood
Often there is a lack of any facial expression.
Adolescence
The face is usually wide at the forehead and tapers to a chin that is pointed. Features of the face become sharper as well as the eyes become less perceptible. The neck elongates revealing additional folds of skin – webbed neck or neck that is prominent – trapezuius – muscles.
Adulthood
When an individual with this syndrome becomes an adult, the crease running from the edge of the nose to the corner of the mouth is prominent and the skin can appear transparent and be wrinkled.
Heart disease
Approximately 80% of individuals with this syndrome have heart disease that is congenital, which accounts for some of the key symptoms and signs. Pediatric cardiologists are normally the first physicians to see those with Noonan syndrome. Several types of heart disease that are congenital and linked with this disorder include:
Disorders with valve
Pulmonary valve stenosis is the narrowing of the pulmonary valve, which is the tissue flap separating the right lower chamber or ventricle of the heart from the pulmonary artery that supplies blood to the lungs. This is the most common problem with the heart seen with this syndrome.
Heart muscle thickening – hypertrophic cardiomyopathy
Abnormal thickening or growth of the heart muscle – affects 20% of those with Noonan syndrome.
Other defects
Individuals with this syndrome frequently have structural problems of the heart. These defects include a hole in the wall which splits up the lower 2 chambers of the heart – ventricular septal defect, or another condition causing arteries to narrow – pulmonary artery stenosis.
Growth problems
The child’s birth weight will more than likely be normal but many of these children have problems with feeding causing poor gain of weight until about 18 months old. The spurt of growth that is normally seen during adolescence could be delayed in the child with this syndrome but since this disease makes bone maturity delayed, the child has the probability for growth to continue into the 20s.
Issues with musculoskeletal
Often individuals with Noonan syndrome have chests that are unusually shaped with a sternum that is sunken or raised. A short neck as well as wide-set nipples with webbed neck is also common.
Disabilities with learning
Intelligence is not affected with this syndrome but there is an amplified risk of learning disabilities. But, it is not unusual for individuals to finish high school, go to college and have careers.
Eye problems
These are abnormalities of the eyelids and the eyes. Trademark features are differences in the size and shape of the eyes. The iris may be green or pale blue. There can be problems with the muscles of the eye, refractive problems, movement of the eyes that is rapid and problems with the eye nerves.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
Bleeding
Individuals with this syndrome have a history of bleeding or bruising that is abnormal.
Problems with the lymphatic system
This system drains fluid that is excess from the body and aids in fighting infection. The problem that is most common is fluid that is excessive on the top of the feet or the back of the hands.
Kidney and genital problems
Most individuals particular males with this syndrome have problems with genitals as well as kidneys.
Problems with skin
These are varied and include the texture or color of the skin. Those with this syndrome can have coarse, curly hair or hair that is sparse.
The treatment of the complications as well as the symptoms which develop with this syndrome hinge on the type as well as the severity. Most issues are treated the same way they are in the population generally.
The approach that might be recommended to deal with various problems with this syndrome can consist of:
Heart treatment
Some drugs can be very effective in the treatment of different types of heart problems. Surgery can be necessary if there is valve involvement.
Treating low growth rate
The child’s height needs to be checked 3 times each year until they are 3 years old and then once each year until adulthood. The physician will need to check the child’s thyroid function, blood chemistry, hormone levels as well as bone growth. If the growth hormone levels are not sufficient, growth hormone therapy can be a management option.
Disabilities with learning
This covers a varied range of behavioral as well as mental issues. Ask the physician about infant stimulation programs.
Vision
The child will need regular exams every 2 years. Most issues with the eye can be treated with glasses alone.
Treatment for bruising and bleeding
If there is a history, avoid aspirin and products that contain aspirin.
Treatment of urinary tract and genital problems
With males if there are undescended testicles at birth, the physician will refer you to a surgeon to decide whether surgery is suitable.
With urinary tract infection – treatment is with antibiotics.
The prognosis of the syndrome is dependent largely on how extensive the varied medical difficulties are, especially the defects of the heart. Individuals who have a severe type of this condition can have a life span that is greatly shorter than those with minor problems. Additionally, occurrence of mental deficit in 25% of individuals will affect any long term prognosis.
Life expectancy depends on the complications involved during the life of an individual with this syndrome as well as the severity of those complications. Limited studies of health-event patterns submit that life expectancy is reduced by approximately 10 years.



What is Noonan Syndrome?
This is a disorder that is caused by a mutation that is genetic and stops the usual development in varied areas of the body. This syndrome can affect an individual in varied way such as:
- Facial characteristics that are unusual
- Stature is short
- Defects of the heart
- Other problems physically
- Possible low intelligence
This syndrome occurs when the fetus receives a copy of the gene that is affected from one parent. This is known as “dominant inheritance”. It may occur also as a mutation that is spontaneous, which means that there is no history of this disorder in the family.
There is currently no precise treatment for this syndrome. Treatment is focused on managing the disorder’s symptoms as well as difficulties that can arise. Growth hormone can be needed to manage short stature in certain individuals with this syndrome.
Noonan Syndrome Symptoms
Facial features
The way an individual’s face appears is one of the main clues which leads to the diagnosis of this syndrome. These appearances or signs alter with age:
Early infancy
When the baby is younger than one month old, it can have eyes that are down-slanting and wide set, ears that are low-set, groove that is deep and peaks that are wide in the upper lip, neck that is short as well as a hairline that is low in the back.
Infancy
The baby can have eyes that are prominent that slant downward as well as lids that are thickened and a nose depressed at the top with a base that is wide and a tip that is bulbous.
Childhood
Often there is a lack of any facial expression.
Adolescence
The face is usually wide at the forehead and tapers to a chin that is pointed. Features of the face become sharper as well as the eyes become less perceptible. The neck elongates revealing additional folds of skin – webbed neck or neck that is prominent – trapezuius – muscles.
Adulthood
When an individual with this syndrome becomes an adult, the crease running from the edge of the nose to the corner of the mouth is prominent and the skin can appear transparent and be wrinkled.
Heart disease
Approximately 80% of individuals with this syndrome have heart disease that is congenital, which accounts for some of the key symptoms and signs. Pediatric cardiologists are normally the first physicians to see those with Noonan syndrome. Several types of heart disease that are congenital and linked with this disorder include:
Disorders with valve
Pulmonary valve stenosis is the narrowing of the pulmonary valve, which is the tissue flap separating the right lower chamber or ventricle of the heart from the pulmonary artery that supplies blood to the lungs. This is the most common problem with the heart seen with this syndrome.
Heart muscle thickening – hypertrophic cardiomyopathy
Abnormal thickening or growth of the heart muscle – affects 20% of those with Noonan syndrome.
Other defects
Individuals with this syndrome frequently have structural problems of the heart. These defects include a hole in the wall which splits up the lower 2 chambers of the heart – ventricular septal defect, or another condition causing arteries to narrow – pulmonary artery stenosis.
Growth problems
The child’s birth weight will more than likely be normal but many of these children have problems with feeding causing poor gain of weight until about 18 months old. The spurt of growth that is normally seen during adolescence could be delayed in the child with this syndrome but since this disease makes bone maturity delayed, the child has the probability for growth to continue into the 20s.
Issues with musculoskeletal
Often individuals with Noonan syndrome have chests that are unusually shaped with a sternum that is sunken or raised. A short neck as well as wide-set nipples with webbed neck is also common.
Disabilities with learning
Intelligence is not affected with this syndrome but there is an amplified risk of learning disabilities. But, it is not unusual for individuals to finish high school, go to college and have careers.
Eye problems
These are abnormalities of the eyelids and the eyes. Trademark features are differences in the size and shape of the eyes. The iris may be green or pale blue. There can be problems with the muscles of the eye, refractive problems, movement of the eyes that is rapid and problems with the eye nerves.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
Bleeding
Individuals with this syndrome have a history of bleeding or bruising that is abnormal.
Problems with the lymphatic system
This system drains fluid that is excess from the body and aids in fighting infection. The problem that is most common is fluid that is excessive on the top of the feet or the back of the hands.
Kidney and genital problems
Most individuals particular males with this syndrome have problems with genitals as well as kidneys.
Problems with skin
These are varied and include the texture or color of the skin. Those with this syndrome can have coarse, curly hair or hair that is sparse.
Noonan Syndrome Treatment
The treatment of the complications as well as the symptoms which develop with this syndrome hinge on the type as well as the severity. Most issues are treated the same way they are in the population generally.
The approach that might be recommended to deal with various problems with this syndrome can consist of:
Heart treatment
Some drugs can be very effective in the treatment of different types of heart problems. Surgery can be necessary if there is valve involvement.
Treating low growth rate
The child’s height needs to be checked 3 times each year until they are 3 years old and then once each year until adulthood. The physician will need to check the child’s thyroid function, blood chemistry, hormone levels as well as bone growth. If the growth hormone levels are not sufficient, growth hormone therapy can be a management option.
Disabilities with learning
This covers a varied range of behavioral as well as mental issues. Ask the physician about infant stimulation programs.
Vision
The child will need regular exams every 2 years. Most issues with the eye can be treated with glasses alone.
Treatment for bruising and bleeding
If there is a history, avoid aspirin and products that contain aspirin.
Treatment of urinary tract and genital problems
With males if there are undescended testicles at birth, the physician will refer you to a surgeon to decide whether surgery is suitable.
With urinary tract infection – treatment is with antibiotics.
Prognosis
The prognosis of the syndrome is dependent largely on how extensive the varied medical difficulties are, especially the defects of the heart. Individuals who have a severe type of this condition can have a life span that is greatly shorter than those with minor problems. Additionally, occurrence of mental deficit in 25% of individuals will affect any long term prognosis.
Noonan Syndrome Life expectancy
Life expectancy depends on the complications involved during the life of an individual with this syndrome as well as the severity of those complications. Limited studies of health-event patterns submit that life expectancy is reduced by approximately 10 years.
Noonan Syndrome Pictures



Relapsing Polychondritis – Pictures, Symptoms, Causes, Diet, Treatment, Prognosis
Relapsing Polychondritis – Pictures, Symptoms, Causes, Diet, Treatment, Prognosis
This is an extremely rare, multisystem disease that may be life-threatening, very difficult to diagnose as well as debilitating. It is categorized by repeated, possibly severe, as well as extremely frightening incidents of inflammation of cartilaginous tissues.
Cartilages that may develop inflammation at various times include nose, ears, joints, windpipe and spine. The heart, blood vessels and eye that all have a biochemical composition that is similar to cartilage, may also be affected.
Ears
Throat – Trachial and Bronchial
Note that early involvement of the throat is usually severe and can be life threatening. An emergency tracheostomy may be needed due to obstruction of the airway.
Intubation or bronchoscopy can cause irritation which leads to airflow reduction. This irritation may take several hours to appear after the procedure. It does not appear to be an occurrence that is frequent but caution is needed after returning home from having such a procedure.
Inflammation of the joints is known as arthritis and causes pain, stiffness of all the joints in the knees, hands, wrist, ankles as well as feet.
With the eye inflammation, it can either be mild to severe and may damage the vision. Cataracts may be triggered by the inflammation or from any cortisone used in treating relapsing polychondritis.
Other areas of tissues that may develop inflammation can include the aorta (leads to aortic valve weakness or aneurysm), tissues around or in the heart (leads to myocarditis and pericarditis), and the skin and the nerves from the brain, (leads to cranial nerve palsies).
The reason or cause of relapsing polychondritis is not known. It is believed that this disease is actually an autoimmunity disorder where the body’s own immunity system that normally fights off foreign invaders into the body, is for some reason misguided. This causes the inflammation to be directed at various healthy tissues in the body.
The list of complications of this disease is almost endless, and some of these include:
A characteristic assortment of symptoms and indications will produce a diagnosis of relapsing polychondritis. Lab tests are often cooperative. Cartilage biopsies of affected area can endorse the diagnosis. Often additional diagnostic tests are done in order to eliminate other conditions that are associated for instance rheumatoid arthritis. Also, it is very important to appraise the airway, but only approximately 10% of individuals will perish from any complications of the airway.
Inflammations which are mild may be treated by aspirin or non-steroidal anti-inflammatory drugs also known as NSAIDs like ibuprofen. Corticosteroids – usually prednisone – are normally prescribed for conditions that are more advanced and they do help with the illness.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
Oral corticosteroids are considered the mainstay for treatment of this illness. Preliminary doses of prednisone range from 0.5 to 1.0 mg/kg depending on the specific problems at presentation. They might have to be sustained over extensive time periods, in which case the use needs to be watched closely to avoid any difficulties.
Immune suppression with:
is usually reserved for cases which are more aggressive.
A chest that is collapsed or collapsed airway may need surgical maintenance and an aorta or a heart valve can need replacing or repair.
When relapsing polychondritis is linked with a systemic vasculitis, the treatment needs to be tailored to the underlying arteritis. Chronic care of the individual with this disorder requires periodic reassessment of the pulmonary, cardiovascular as well as renal systems.
While medical therapy that is conventional can help to relieve symptoms of relapsing polychondritis these treatments do not report the root of the problem. Normally, by undergoing wide-ranging natural medication testing, the reason that the body is producing the antibodies against itself can be discovered. It is believed that the reasons include allergies or sensitivities to foods, chemicals, infections and various inhalants.
There is currently no known cure for this disease. It only can be fought as indicated by each case of inflammation as well as deterioration of cartilaginous tissue. As this illness progresses over a period of years, the rate of mortality increases. At 5 years duration, relapsing polychondritis has a 30% rate of mortality.
On the internet there are several websites with individuals who have had this disease and have responded to nutritional strategies and responded well. A diet referred to as the McDougall Program is recommended by many as the best as well as the most practical. There is a book available under this name. The diet is basically a low-fat vegan diet, which means the elimination of all dairy products and eggs as well as the elimination of meat, fish and chicken. Many of the autoimmune diseases have responded favorably to this type of diet.
In short – try a “no animal proteins” in any form diet.



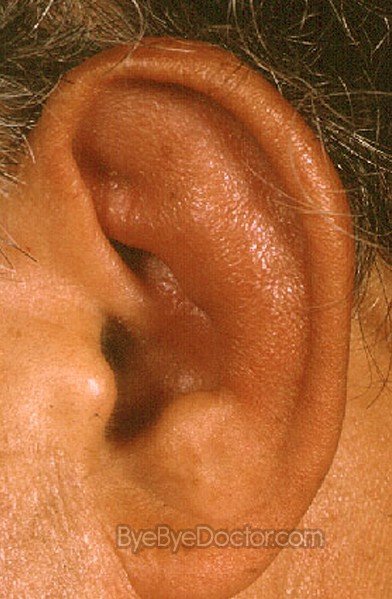
What is Relapsing Polychondritis?
This is an extremely rare, multisystem disease that may be life-threatening, very difficult to diagnose as well as debilitating. It is categorized by repeated, possibly severe, as well as extremely frightening incidents of inflammation of cartilaginous tissues.
Cartilages that may develop inflammation at various times include nose, ears, joints, windpipe and spine. The heart, blood vessels and eye that all have a biochemical composition that is similar to cartilage, may also be affected.
Relapsing Polychondritis Symptoms
Ears
- Redness
- Pain
- Cauliflower ear
- Loss of hearing
Throat – Trachial and Bronchial
- Hoarseness
- Coughing
- Redness in upper chest area
- Pain
- Shortness breath
- Trouble breathing
- Choking
Note that early involvement of the throat is usually severe and can be life threatening. An emergency tracheostomy may be needed due to obstruction of the airway.
Intubation or bronchoscopy can cause irritation which leads to airflow reduction. This irritation may take several hours to appear after the procedure. It does not appear to be an occurrence that is frequent but caution is needed after returning home from having such a procedure.
- Joints – General pain with or without swelling
- Sinus/Nose – Deterioration (saddle nose), blockage of sinuses, severe and frequent sinus headaches. Fall is normally slow to the point of not being noticed until compared to some old photos.
- Vision – Vision is blurred, headaches, episcleritis, or scleritis
Inflammation of the joints is known as arthritis and causes pain, stiffness of all the joints in the knees, hands, wrist, ankles as well as feet.
With the eye inflammation, it can either be mild to severe and may damage the vision. Cataracts may be triggered by the inflammation or from any cortisone used in treating relapsing polychondritis.
Other areas of tissues that may develop inflammation can include the aorta (leads to aortic valve weakness or aneurysm), tissues around or in the heart (leads to myocarditis and pericarditis), and the skin and the nerves from the brain, (leads to cranial nerve palsies).
Relapsing Polychondritis Causes
The reason or cause of relapsing polychondritis is not known. It is believed that this disease is actually an autoimmunity disorder where the body’s own immunity system that normally fights off foreign invaders into the body, is for some reason misguided. This causes the inflammation to be directed at various healthy tissues in the body.
The list of complications of this disease is almost endless, and some of these include:
- Loss of hearing in cases that are recurring
- Weakness of the aortic valve
- Aneurysm
- Death
Relapsing Polychondritis Treatment
A characteristic assortment of symptoms and indications will produce a diagnosis of relapsing polychondritis. Lab tests are often cooperative. Cartilage biopsies of affected area can endorse the diagnosis. Often additional diagnostic tests are done in order to eliminate other conditions that are associated for instance rheumatoid arthritis. Also, it is very important to appraise the airway, but only approximately 10% of individuals will perish from any complications of the airway.
Inflammations which are mild may be treated by aspirin or non-steroidal anti-inflammatory drugs also known as NSAIDs like ibuprofen. Corticosteroids – usually prednisone – are normally prescribed for conditions that are more advanced and they do help with the illness.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
Oral corticosteroids are considered the mainstay for treatment of this illness. Preliminary doses of prednisone range from 0.5 to 1.0 mg/kg depending on the specific problems at presentation. They might have to be sustained over extensive time periods, in which case the use needs to be watched closely to avoid any difficulties.
Immune suppression with:
- Cyclophosphamide
- Cyclosporine
- Azathioprine
- Dapsone
is usually reserved for cases which are more aggressive.
A chest that is collapsed or collapsed airway may need surgical maintenance and an aorta or a heart valve can need replacing or repair.
When relapsing polychondritis is linked with a systemic vasculitis, the treatment needs to be tailored to the underlying arteritis. Chronic care of the individual with this disorder requires periodic reassessment of the pulmonary, cardiovascular as well as renal systems.
While medical therapy that is conventional can help to relieve symptoms of relapsing polychondritis these treatments do not report the root of the problem. Normally, by undergoing wide-ranging natural medication testing, the reason that the body is producing the antibodies against itself can be discovered. It is believed that the reasons include allergies or sensitivities to foods, chemicals, infections and various inhalants.
Prognosis
There is currently no known cure for this disease. It only can be fought as indicated by each case of inflammation as well as deterioration of cartilaginous tissue. As this illness progresses over a period of years, the rate of mortality increases. At 5 years duration, relapsing polychondritis has a 30% rate of mortality.
Diet
On the internet there are several websites with individuals who have had this disease and have responded to nutritional strategies and responded well. A diet referred to as the McDougall Program is recommended by many as the best as well as the most practical. There is a book available under this name. The diet is basically a low-fat vegan diet, which means the elimination of all dairy products and eggs as well as the elimination of meat, fish and chicken. Many of the autoimmune diseases have responded favorably to this type of diet.
In short – try a “no animal proteins” in any form diet.
Relapsing Polychondritis Pictures



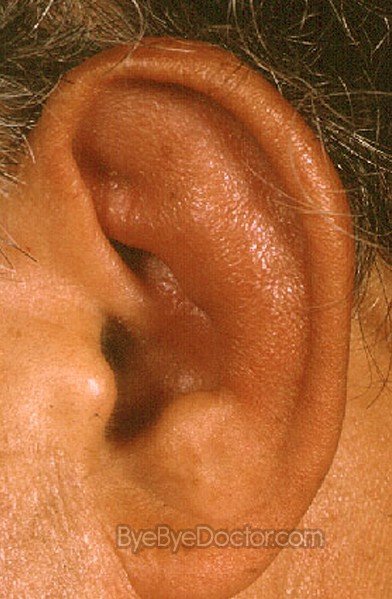
Merkel Cell Carcinoma – Symptoms, Treatment, Staging, Prognosis, Pictures
Merkel Cell Carcinoma – Symptoms, Treatment, Staging, Prognosis, Pictures
This is a very rare kind of cancer of the skin that normally appears as a bluish-red or flesh colored nodule. It often appears on the face, neck or head. Merkel cell cancer is also referred to as “neuroendocrine carcinoma of the skin”.
Merkel cell cancer often grows in older adults. Long-time exposure to the sun or a weakened immune system can increase the threat of this form of cancer.
Merkel cell cancer is prone to grow quickly and to also spread swiftly to other areas of the body. Options for treatment of this type of cancer normally are contingent on if the cancer has developed away from the skin.
The first symptom of this type of cancer is normally a very fast growing nodule or tumor that is painless and is developing on the skin. This shiny nodule can be skin colored or may appear is shades of blue, purple or red. Most Merkel cell lesions develop on the head, neck or face but they also can develop anywhere on the body, even in areas not open to sunlight.
If a freckle, mole or bump is noticed that is beginning to change shape, color or size and is rapidly growing as well as bleeds easily after any minor trauma for instance washing the skin or shaving – it is time to make an appointment with the primary care physician.
Treatments for this type of cancer may include:
Surgery
With surgery, the physician will remove the tumor together with the surrounding skin border that is normal and circles the tumor. If any evidence shows that this cancer has migrated to lymphatic nodes in the region of the tumor, then these lymphatic nodes are also removed in a procedure known as “lymph node dissection”.
The physician most like will use a type of scalpel to cut the cancer away. In many cases, the physician might use a technique called Mohs micrographic surgery. Once the visible part of the tumor has been removed, the physician makes very thin slices of the tumor tissue to examine the slices under a microscope. This process is repeated until the cancer cells no longer are found in the tissue of a slice. This kind of procedure takes away less tissue that is normal tissue – reducing scarring – and it guarantees a tumor free boundary of skin. Mohs surgery is frequently used for cancer on the face.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
Radiation therapy
This comprises guiding high energy beams, such as x-rays at cancer cells. During this type of treatment, the individual is situated on a table and a very large machine travels around the individual, guiding the beams to very precise points on the body.
The therapy is often used after surgery to eradicate any cancer cells that might remain after the removal of the tumor. Because of the rarity of Merkel cell cancer, it is not clearly precise who should obtain this therapy after total surgical removal of the lesion. Discuss with the physician the benefits as well as the cons of having radiation therapy after the removal of the cancer.
This option also can be used to shrivel the cancer before it is removed or as the sole option for treatment in those individuals who choose no surgery. Radiation also can be used to treat any areas where the cancer has spread.
Chemotherapy
This is the using of drugs to kill the cells of cancer. Chemotherapy drugs are normally administrated thru IV or may be taken oral or both.
The doctor can commend chemotherapy if the cancer spreads to the lymphatic nodes or other organs in the body, or if it returns despite treatment. But, whether chemotherapy improves the rate of survival in those individuals with Merkel cell carcinoma is still unclear. Discuss with the physician the benefits as well as the risks of using chemotherapy.
Stages I and II of this type cancer are described as localized disease of the skin at the primary site. Stage I is for those primary lesions that are less than or equal to 2 centimeters and stage II is for lesions that are primary and or greater than 2 centimeters. Stage III is described as disease which involves any nearby lymphatic nodes or regional lymph nodes. Stage IV of the disease is found beyond the regional lymphatic nodes.
The majority of deaths from this cancer happen within the first 3 years of diagnosis. Those individuals with stage I, II and III disease do much better than individuals with stage IV disease which is metastatic. A new study shows that individuals who have no lymphatic node involvement have an excellent prognosis.




What is Merkel Cell Carcinoma?
This is a very rare kind of cancer of the skin that normally appears as a bluish-red or flesh colored nodule. It often appears on the face, neck or head. Merkel cell cancer is also referred to as “neuroendocrine carcinoma of the skin”.
Merkel cell cancer often grows in older adults. Long-time exposure to the sun or a weakened immune system can increase the threat of this form of cancer.
Merkel cell cancer is prone to grow quickly and to also spread swiftly to other areas of the body. Options for treatment of this type of cancer normally are contingent on if the cancer has developed away from the skin.
Merkel Cell Carcinoma Symptoms
The first symptom of this type of cancer is normally a very fast growing nodule or tumor that is painless and is developing on the skin. This shiny nodule can be skin colored or may appear is shades of blue, purple or red. Most Merkel cell lesions develop on the head, neck or face but they also can develop anywhere on the body, even in areas not open to sunlight.
If a freckle, mole or bump is noticed that is beginning to change shape, color or size and is rapidly growing as well as bleeds easily after any minor trauma for instance washing the skin or shaving – it is time to make an appointment with the primary care physician.
Merkel Cell Carcinoma Treatment
Treatments for this type of cancer may include:
Surgery
With surgery, the physician will remove the tumor together with the surrounding skin border that is normal and circles the tumor. If any evidence shows that this cancer has migrated to lymphatic nodes in the region of the tumor, then these lymphatic nodes are also removed in a procedure known as “lymph node dissection”.
The physician most like will use a type of scalpel to cut the cancer away. In many cases, the physician might use a technique called Mohs micrographic surgery. Once the visible part of the tumor has been removed, the physician makes very thin slices of the tumor tissue to examine the slices under a microscope. This process is repeated until the cancer cells no longer are found in the tissue of a slice. This kind of procedure takes away less tissue that is normal tissue – reducing scarring – and it guarantees a tumor free boundary of skin. Mohs surgery is frequently used for cancer on the face.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
Radiation therapy
This comprises guiding high energy beams, such as x-rays at cancer cells. During this type of treatment, the individual is situated on a table and a very large machine travels around the individual, guiding the beams to very precise points on the body.
The therapy is often used after surgery to eradicate any cancer cells that might remain after the removal of the tumor. Because of the rarity of Merkel cell cancer, it is not clearly precise who should obtain this therapy after total surgical removal of the lesion. Discuss with the physician the benefits as well as the cons of having radiation therapy after the removal of the cancer.
This option also can be used to shrivel the cancer before it is removed or as the sole option for treatment in those individuals who choose no surgery. Radiation also can be used to treat any areas where the cancer has spread.
Chemotherapy
This is the using of drugs to kill the cells of cancer. Chemotherapy drugs are normally administrated thru IV or may be taken oral or both.
The doctor can commend chemotherapy if the cancer spreads to the lymphatic nodes or other organs in the body, or if it returns despite treatment. But, whether chemotherapy improves the rate of survival in those individuals with Merkel cell carcinoma is still unclear. Discuss with the physician the benefits as well as the risks of using chemotherapy.
Merkel Cell Carcinoma Staging
Stages I and II of this type cancer are described as localized disease of the skin at the primary site. Stage I is for those primary lesions that are less than or equal to 2 centimeters and stage II is for lesions that are primary and or greater than 2 centimeters. Stage III is described as disease which involves any nearby lymphatic nodes or regional lymph nodes. Stage IV of the disease is found beyond the regional lymphatic nodes.
Prognosis
The majority of deaths from this cancer happen within the first 3 years of diagnosis. Those individuals with stage I, II and III disease do much better than individuals with stage IV disease which is metastatic. A new study shows that individuals who have no lymphatic node involvement have an excellent prognosis.
Merkel Cell Carcinoma Pictures




Sacroiliitis
Sacroiliitis
Sacroiliitis is an orthopedic medical condition involving the inflammation of the sacroiliac joints, the medical term referring to either one of the joints on both sides of the body that link the lower ends of the spine to the pelvic bone. The condition is one that entails a considerable amount of pain located in the lower regions of the back due to the internal irritation of the joint structure. The pain experienced by patients with sacroiliitis is also easily exacerbated by several aggravating activities that apply pressure or force upon the sacroiliac joints, such as standing for long periods of time for example. The disorder is classified under the family of diseases referred to as spondyloarthropathies, which includes any medical condition that results in the inflammation of any region of the spine’s structure.
The condition is not easily distinguishable from other sources of pain in the lower back as sacroiliitis shares its symptoms with various other conditions, but adequately thorough diagnostic testing can determine the existence of the condition. Once diagnosed, the condition can be treated through a full regimen consisting of combined efforts of drugs, rest, and physical therapy. Detection and treatment is especially important as the condition can produce severe complications if the irritation is not resolved.
The central feature of sacroiliitis is the pain that accompanies the condition. The pain is distinguished due to its nature of being localized in the region of lower back as well as in the buttocks in certain instances. The following are the specific characteristics of sacroiliitis.
If the sacroiliitis is able to progress, complications may develop. Watch out for symptoms such as difficulty breathing, heart problems, or difficulty with posture and gait as these are possible signs of complications of the illness.
The disorder can be caused by several possible factors, each one affecting the sacroiliac joints in a way. A possible source of the irritation in the sacroiliac joints can be brought about by sustaining an injury to the area. Common triggers of the sacroiliitis can come in the form of a vehicular accident or even a simple fall. Any extreme force applied to the sacroiliac joints can cause injury to the connective tissues in the region, impairing their ability to be fully made use of in movement and support.
Osteoarthritis as a part of the process of aging can also bring about the irritation. The mechanism of the condition is similar to that of any physical trauma, involving the destruction of tissues in the joints necessary to maintain the body’s mobility.
Some pregnant women may also experience sacroiliitis as a consequence of the physical changes a woman’s body undergoes during pregnancy. Over the period of the 9 months it takes for a baby to fully develop within the mother’s womb, the mother’s own body adjusts to the presence of the new life by adapting. These adjustments involve the stretching of the sacroiliac joints in order to allow the accommodation of the baby during childbirth. These changes in the bone structure of the woman’s hips are not meant to produce debilitating results, but in combination with the woman’s increased weight, the already loosened joints may suffer from the increased pressure and become worn out.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
In addition to all the previously mentioned causes, infection is another possible source of sacroiliitis. The bacterial growth may be one that was able to migrate from an originally different location, eventually reaching the joints of the sacrum and the pelvis and proceeding with their proliferation in this location.
Treatment for sacroiliitis is aimed at controlling symptoms and eliminating the source of the irritation in order to improve and recover the utility of sacroiliac joints. Several types of drugs are prescribed by doctors to address the symptoms of the condition. Pain relievers are an obvious element in the course of treatment to get rid of the severe pain. Over-the-counter painkillers can be used but if pain is much too great and is unresolved by these, the doctor can prescribe stronger analgesics such as tramadol, for instance. Some doctors may prescribe narcotics for extreme pain but these are used cautiously and only for short periods of time as patients can develop addictions to these medications.
Injectable drugs are also used for patients. These include betamethasone or triamcinolone. The medications are injected directly into the affected joints to reduce inflammation and subsequently help with pain as well. These shots are however limited to only a few per year as they can eventually be unhealthy for the bones if used continuously.
Physical therapy is also necessary for patients with sacroiliitis. These consist of range-of-motion exercises and stretching routines to improve the joints’ performance and endurance. These are especially necessary if the sacroiliitis has already produced degradation in the patient’s ability to tolerate physical activity.
Because sacroiliitis can often be difficult to distinguish from other causes of lower back pain, imaging tests are necessary to obtain an internal view of the bone structure to verify the presence of an inflammation. The most basic imaging test used is the x-ray, which is usually enough to detect the presence of irritation and inflammation in the sacroiliac joints. More comprehensive and detailed imaging tests however are also available; these include CT scans and MRIs which produce cross-sectional images of the internal structure of the bones, allowing more in depth observation.
Recovery for patients suffering from sacroiliitis will vary depending on the severity of the condition as well as the patient’s ability to religiously comply with his or her treatment regimen. Ideally, once treatment for the condition has begun, the pain may be resolved within a short period of a few days. In other instances, the pain may take several weeks to disappear, typically taking 2 or 3 weeks.
What is Sacroiliitis?
Sacroiliitis is an orthopedic medical condition involving the inflammation of the sacroiliac joints, the medical term referring to either one of the joints on both sides of the body that link the lower ends of the spine to the pelvic bone. The condition is one that entails a considerable amount of pain located in the lower regions of the back due to the internal irritation of the joint structure. The pain experienced by patients with sacroiliitis is also easily exacerbated by several aggravating activities that apply pressure or force upon the sacroiliac joints, such as standing for long periods of time for example. The disorder is classified under the family of diseases referred to as spondyloarthropathies, which includes any medical condition that results in the inflammation of any region of the spine’s structure.
The condition is not easily distinguishable from other sources of pain in the lower back as sacroiliitis shares its symptoms with various other conditions, but adequately thorough diagnostic testing can determine the existence of the condition. Once diagnosed, the condition can be treated through a full regimen consisting of combined efforts of drugs, rest, and physical therapy. Detection and treatment is especially important as the condition can produce severe complications if the irritation is not resolved.
Sacroiliitis Symptoms
The central feature of sacroiliitis is the pain that accompanies the condition. The pain is distinguished due to its nature of being localized in the region of lower back as well as in the buttocks in certain instances. The following are the specific characteristics of sacroiliitis.
- Pain, generally occurring in the lower back or buttocks
- Pain may also radiate to the lower limbs, affecting the groin, legs, or the feet
- Difficulty engaging in some types of activity such as sitting, standing, walking, and bending
- Pain is exacerbated by several activities, such as standing for long periods of time, climbing stairs, running, and focusing one’s weight on one side of the body by supporting oneself up more on one leg. Generally any action that requires increased force and effort from the sacroiliac joints stirs up the painful sensations.
If the sacroiliitis is able to progress, complications may develop. Watch out for symptoms such as difficulty breathing, heart problems, or difficulty with posture and gait as these are possible signs of complications of the illness.
Sacroiliitis Causes
The disorder can be caused by several possible factors, each one affecting the sacroiliac joints in a way. A possible source of the irritation in the sacroiliac joints can be brought about by sustaining an injury to the area. Common triggers of the sacroiliitis can come in the form of a vehicular accident or even a simple fall. Any extreme force applied to the sacroiliac joints can cause injury to the connective tissues in the region, impairing their ability to be fully made use of in movement and support.
Osteoarthritis as a part of the process of aging can also bring about the irritation. The mechanism of the condition is similar to that of any physical trauma, involving the destruction of tissues in the joints necessary to maintain the body’s mobility.
Some pregnant women may also experience sacroiliitis as a consequence of the physical changes a woman’s body undergoes during pregnancy. Over the period of the 9 months it takes for a baby to fully develop within the mother’s womb, the mother’s own body adjusts to the presence of the new life by adapting. These adjustments involve the stretching of the sacroiliac joints in order to allow the accommodation of the baby during childbirth. These changes in the bone structure of the woman’s hips are not meant to produce debilitating results, but in combination with the woman’s increased weight, the already loosened joints may suffer from the increased pressure and become worn out.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
In addition to all the previously mentioned causes, infection is another possible source of sacroiliitis. The bacterial growth may be one that was able to migrate from an originally different location, eventually reaching the joints of the sacrum and the pelvis and proceeding with their proliferation in this location.
Sacroiliitis Treatment
Treatment for sacroiliitis is aimed at controlling symptoms and eliminating the source of the irritation in order to improve and recover the utility of sacroiliac joints. Several types of drugs are prescribed by doctors to address the symptoms of the condition. Pain relievers are an obvious element in the course of treatment to get rid of the severe pain. Over-the-counter painkillers can be used but if pain is much too great and is unresolved by these, the doctor can prescribe stronger analgesics such as tramadol, for instance. Some doctors may prescribe narcotics for extreme pain but these are used cautiously and only for short periods of time as patients can develop addictions to these medications.
Injectable drugs are also used for patients. These include betamethasone or triamcinolone. The medications are injected directly into the affected joints to reduce inflammation and subsequently help with pain as well. These shots are however limited to only a few per year as they can eventually be unhealthy for the bones if used continuously.
Exercises
Physical therapy is also necessary for patients with sacroiliitis. These consist of range-of-motion exercises and stretching routines to improve the joints’ performance and endurance. These are especially necessary if the sacroiliitis has already produced degradation in the patient’s ability to tolerate physical activity.
Diagnosis
Because sacroiliitis can often be difficult to distinguish from other causes of lower back pain, imaging tests are necessary to obtain an internal view of the bone structure to verify the presence of an inflammation. The most basic imaging test used is the x-ray, which is usually enough to detect the presence of irritation and inflammation in the sacroiliac joints. More comprehensive and detailed imaging tests however are also available; these include CT scans and MRIs which produce cross-sectional images of the internal structure of the bones, allowing more in depth observation.
Prognosis
Recovery for patients suffering from sacroiliitis will vary depending on the severity of the condition as well as the patient’s ability to religiously comply with his or her treatment regimen. Ideally, once treatment for the condition has begun, the pain may be resolved within a short period of a few days. In other instances, the pain may take several weeks to disappear, typically taking 2 or 3 weeks.
Subscribe to:
Comments (Atom)