Adenomyosis – Symptoms, Treatment, Pictures, Causes, Diagnosis, Diet
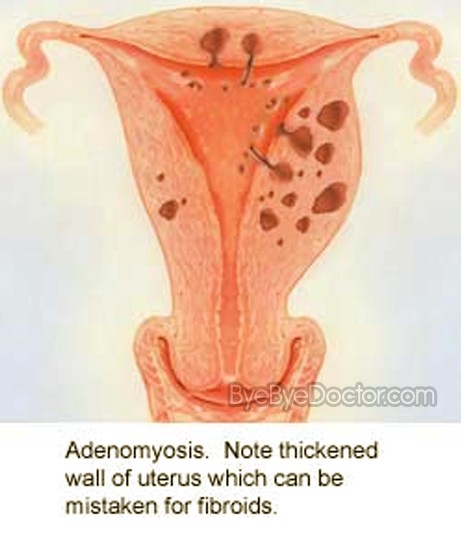
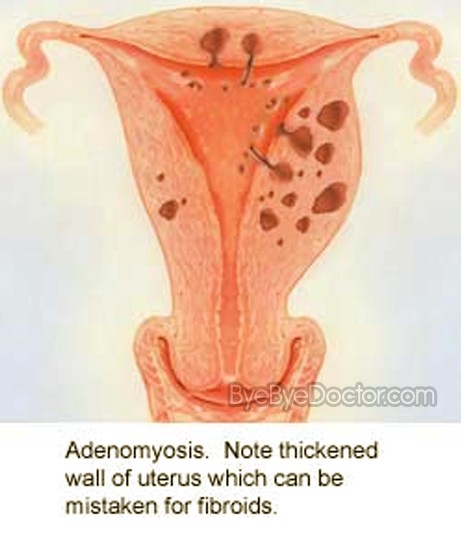
This is a disorder where the endometrial tissue lining the walls of the uterus exists inside and grows into the muscles of the walls of the uterus. Or in other words, the lining of the uterus becomes thickened and grows into the outer muscular walls of the uterus. This disorder occurs mostly in the late stages of the childbearing years as well as after the woman has had children.
This disease is not like endometriosis – which is a condition where the lining of the uterus can become implanted in areas of the body exteriorly from the uterus – though many with adenomyosis also often have endometriosis. What causes adenomyosis is not known, but the illness normally vanishes after a woman is in post-menopause. For those women who have the more severe pain from this disease, there are opportunities for treatments which may help but the only total cure is to have a hysterectomy.
Although this condition can be very painful, adenomyosis is normally harmless.
Adenomyosis is often called “silent” because with some women it causes no symptoms or signs and only causes mild discomfort. But in other women the following symptoms and signs can be experienced:
A woman’s uterus can increase to almost double or even triple its regular size. Although a woman may not know that the uterus is inflated, she might notice that the lower abdomen does feel tender or seem bigger.
If a woman experiences any of the symptoms or signs of adenomyosis, like heavy, prolonged bleeding during her periods or cramping which is severe and interferes with normal activities, then it is time to schedule a visit to see her primary care physician or her gynecologist.
Causes of this disease are not known. Theories put forth by experts on a likely cause include:
Tissue growth which is invasive
There are many experts who accept as true that adenomyosis is caused by the direct interference of endometrial cells starting at the exterior of the lining of the uterus into the muscles which form the walls of the uterus. Incisions made into the uterus during any surgery such as a C-section encourages the direct incursion of the cells of the endometrium into the uterus wall.
Developmental origins
There are other medical professionals who believe that adenomyosis starts within the muscle of the uterus from endometrial tissue which was placed there once the uterus was originally formed in the fetus of females.
Uterine inflammation caused by childbirth
There is an alternative theory which advocates an association between childbirth and adenomyosis. Uterine lining inflammation during the period called postpartum could create a breakdown in the regular borderline of cells in the uterine lining.
No matter what is the cause of adenomyosis or why it develops, its development rest on the flowing estrogen in the woman’s body. When the production of estrogen declines as menopause begins, adenomyosis normally vanishes.
The risk aspects for adenomyosis can include:
Pain and extreme bleeding is not harmful but adenomyosis can have a very adverse effect on a person’s lifestyle. The woman may find herself evading activities which she enjoyed previously – but now she has no idea where or when she might begin bleeding. Periods which are painful can cause missed school or work and can put a strain on relationships. Any periodic pain can eventually lead to irritability, depression, anger, feelings of powerlessness and anxiety. This is why it is so important that any woman with these symptoms seek medical diagnosis and treatment if she believes that she could have adenomyosis.
If a woman experiences heavy, prolonged bleeding, prolonged anemia could result.
The physician may be suspicious of adenomyosis based on the following:
In some rare instances, the physician may do a biopsy of the endometrial tissue which is just a section of the cells from the lining of the uterus to test. By testing the physician can verify that the abnormal uterine bleeding is not linked with any further problems which could be serious.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
But it needs to be noted that this biopsy will not help the physician endorse the diagnosis of adenomyosis. The lone method to ensure an adenomyosis diagnosis is to examine the uterine tissue using a microscope – but only after a hysterectomy removal of the uterus.
There are other diseases of the uterus which many women can have which causes the symptoms and signs to be comparable to adenomyosis thus making adenomyosis much more problematic to diagnose. Some of these conditions comprise uterine cell growth outside the uterus in other areas of the pelvic cavity (endometriosis), fibroid tumors (leiomyomas), as well as growths in the lining of the uterus (endometrial polyps). A physician can only diagnose adenomyosis after eliminating any other reasons for the symptoms or signs.
Testing of the blood will not indicate whether a woman has adenomyosis, but her physician may advise testing to assess the amount of menstrual blood which is lost.
Normally adenomyosis goes away following menopause, so management can depend on how close to that phase of life you are.
Options for treatment of adenomyosis include:
Anti-inflammatory drugs
If you are nearing menopause, the physician may suggest you use anti-inflammatory drugs, such as Advil, Motrin as well as others to manage pain. Beginning anti-inflammatory medications 2 to 3 days before the beginning of your period and continuing to take it during the period, the amount of menstrual blood flow can be reduced as well as relieving the pain.
Hormone drugs
By controlling the menstrual cycle thru joint “estrogen-progestin” oral birth control or thru patches or vaginal rings containing hormones can lessen the pain and heavy bleeding linked with adenomyosis. Contraception which is progestin-only, such as an intrauterine device containing progestin or a birth control pill which is continuous-use often can lean to amenorrhea or the lack of menstrual periods and can offer relief.
Hysterectomy
If the pain is very serious and menopause is some years off, the physician can recommend surgical removal the uterus. Removing the ovaries is not needed to control this condition.
In order to decrease cramping as well as pelvic pain which is linked to adenomyosis, there are self-care procedures which include:
There are certain changes in diet which can lead to women having few problems with Adenomyosis. This diet includes plenty of:
Avoid totally:
These are significant changes. The benefits of this diet are reduced menstrual cramps, incredibly easy weight loss and increased energy. In fact for many the diet changes are so very rewarding that many will wish they had tried it sooner.
Calcium Balance
There are other dietary changes that also can help. For example, the addition of calcium, vitamin B6, essential fatty acids and others. Evidence has shown that getting into a better calcium balance can help reduce both menstrual pain as well as PMS. If calcium does not completely relieve the symptoms, it will at least help with milder symptoms.
Studies have been done with women taking calcium carbonate supplement – 1000 milligrams per day. The amount of calcium which is loss can be cut to less than half or further reduced by:
Vitamin B6
This has been shown to reduce pain in some research studies. It seems to work by increasing the production of neurotransmitters which inhibit the sensations of pain. It also appears to play some role in controlling estrogens by helping their removal from the liver. The usual dose is in the range of 50-150 milligrams per day.
Essential Fatty Acids
Prostaglandins are involved in muscle contractions and menstrual pain and the fat that has the most prostaglandins are more beneficial. Omega-3 fatty acids seem to have the most anti-inflammatory properties rather than other fats. Some women adjust their fat balance by adding extra omega 3 rich oils such as flax oil to the diet. This counteracts the bad fats from meats and dairy products.

What is Adenomyosis?
This is a disorder where the endometrial tissue lining the walls of the uterus exists inside and grows into the muscles of the walls of the uterus. Or in other words, the lining of the uterus becomes thickened and grows into the outer muscular walls of the uterus. This disorder occurs mostly in the late stages of the childbearing years as well as after the woman has had children.
This disease is not like endometriosis – which is a condition where the lining of the uterus can become implanted in areas of the body exteriorly from the uterus – though many with adenomyosis also often have endometriosis. What causes adenomyosis is not known, but the illness normally vanishes after a woman is in post-menopause. For those women who have the more severe pain from this disease, there are opportunities for treatments which may help but the only total cure is to have a hysterectomy.
Although this condition can be very painful, adenomyosis is normally harmless.
Adenomyosis Symptoms
Adenomyosis is often called “silent” because with some women it causes no symptoms or signs and only causes mild discomfort. But in other women the following symptoms and signs can be experienced:
- Prolonged as well as heavy menstrual bleeding
- Piercing, scalpel-like pain in the pelvis as well as severe cramping during menstruation – this is known as dysmenorrhea.
- Cramps which last thru out the period and get worse as the woman ages.
- Pain while having intercourse.
- Passing clots of blood during the period.
- Bleeding in between monthly periods.
A woman’s uterus can increase to almost double or even triple its regular size. Although a woman may not know that the uterus is inflated, she might notice that the lower abdomen does feel tender or seem bigger.
If a woman experiences any of the symptoms or signs of adenomyosis, like heavy, prolonged bleeding during her periods or cramping which is severe and interferes with normal activities, then it is time to schedule a visit to see her primary care physician or her gynecologist.
Adenomyosis Causes
Causes of this disease are not known. Theories put forth by experts on a likely cause include:
Tissue growth which is invasive
There are many experts who accept as true that adenomyosis is caused by the direct interference of endometrial cells starting at the exterior of the lining of the uterus into the muscles which form the walls of the uterus. Incisions made into the uterus during any surgery such as a C-section encourages the direct incursion of the cells of the endometrium into the uterus wall.
Developmental origins
There are other medical professionals who believe that adenomyosis starts within the muscle of the uterus from endometrial tissue which was placed there once the uterus was originally formed in the fetus of females.
Uterine inflammation caused by childbirth
There is an alternative theory which advocates an association between childbirth and adenomyosis. Uterine lining inflammation during the period called postpartum could create a breakdown in the regular borderline of cells in the uterine lining.
No matter what is the cause of adenomyosis or why it develops, its development rest on the flowing estrogen in the woman’s body. When the production of estrogen declines as menopause begins, adenomyosis normally vanishes.
The risk aspects for adenomyosis can include:
- Previous surgery involving the uterus, such as fibroid removal or C-section
- Childbirth
Pain and extreme bleeding is not harmful but adenomyosis can have a very adverse effect on a person’s lifestyle. The woman may find herself evading activities which she enjoyed previously – but now she has no idea where or when she might begin bleeding. Periods which are painful can cause missed school or work and can put a strain on relationships. Any periodic pain can eventually lead to irritability, depression, anger, feelings of powerlessness and anxiety. This is why it is so important that any woman with these symptoms seek medical diagnosis and treatment if she believes that she could have adenomyosis.
If a woman experiences heavy, prolonged bleeding, prolonged anemia could result.
Adenomyosis Diagnosis
The physician may be suspicious of adenomyosis based on the following:
- Symptoms and signs
- Pelvic examination that reveals an uterus which is enlarged and that is tender when touched
- Uterus magnetic resonance imaging or MRI
- Uterus ultrasound image
In some rare instances, the physician may do a biopsy of the endometrial tissue which is just a section of the cells from the lining of the uterus to test. By testing the physician can verify that the abnormal uterine bleeding is not linked with any further problems which could be serious.
http://www.Symptoms-Causes-treatment.blogspot.com detect diseases at an early stage symptoms, and find out the causes and treatments best suited.
But it needs to be noted that this biopsy will not help the physician endorse the diagnosis of adenomyosis. The lone method to ensure an adenomyosis diagnosis is to examine the uterine tissue using a microscope – but only after a hysterectomy removal of the uterus.
There are other diseases of the uterus which many women can have which causes the symptoms and signs to be comparable to adenomyosis thus making adenomyosis much more problematic to diagnose. Some of these conditions comprise uterine cell growth outside the uterus in other areas of the pelvic cavity (endometriosis), fibroid tumors (leiomyomas), as well as growths in the lining of the uterus (endometrial polyps). A physician can only diagnose adenomyosis after eliminating any other reasons for the symptoms or signs.
Testing of the blood will not indicate whether a woman has adenomyosis, but her physician may advise testing to assess the amount of menstrual blood which is lost.
Adenomyosis Treatment
Normally adenomyosis goes away following menopause, so management can depend on how close to that phase of life you are.
Options for treatment of adenomyosis include:
Anti-inflammatory drugs
If you are nearing menopause, the physician may suggest you use anti-inflammatory drugs, such as Advil, Motrin as well as others to manage pain. Beginning anti-inflammatory medications 2 to 3 days before the beginning of your period and continuing to take it during the period, the amount of menstrual blood flow can be reduced as well as relieving the pain.
Hormone drugs
By controlling the menstrual cycle thru joint “estrogen-progestin” oral birth control or thru patches or vaginal rings containing hormones can lessen the pain and heavy bleeding linked with adenomyosis. Contraception which is progestin-only, such as an intrauterine device containing progestin or a birth control pill which is continuous-use often can lean to amenorrhea or the lack of menstrual periods and can offer relief.
Hysterectomy
If the pain is very serious and menopause is some years off, the physician can recommend surgical removal the uterus. Removing the ovaries is not needed to control this condition.
In order to decrease cramping as well as pelvic pain which is linked to adenomyosis, there are self-care procedures which include:
- Soaking in a bath which is warm
- On the abdomen using a heating pad
- Taking OTC anti-inflammatory drugs such as Motrin, Advil or others.
Adenomyosis Diet
There are certain changes in diet which can lead to women having few problems with Adenomyosis. This diet includes plenty of:
- Whole grains – Whole grain bread, brown rice and oatmeal
- Vegetables – Carrots, broccoli, sweet potatoes, spinach, Swiss chard, Brussels sprouts
- Legumes – Peas, lentils and beans
- Fruits
Avoid totally:
- Animal products of any types – poultry, fish, eggs, meats and dairy products
- Added vegetable oils – salad dressings, all cooking oils, margarine
- Any other fatty foods – French fries, doughnuts, potato chips, peanut butter
These are significant changes. The benefits of this diet are reduced menstrual cramps, incredibly easy weight loss and increased energy. In fact for many the diet changes are so very rewarding that many will wish they had tried it sooner.
Calcium Balance
There are other dietary changes that also can help. For example, the addition of calcium, vitamin B6, essential fatty acids and others. Evidence has shown that getting into a better calcium balance can help reduce both menstrual pain as well as PMS. If calcium does not completely relieve the symptoms, it will at least help with milder symptoms.
Studies have been done with women taking calcium carbonate supplement – 1000 milligrams per day. The amount of calcium which is loss can be cut to less than half or further reduced by:
- Avoiding excess sugar and sodium
- Limiting coffee to 2 cups per day
- Avoid tobacco
- Regular exercise
- Vitamin D either from sun or a multiple vitamin
Vitamin B6
This has been shown to reduce pain in some research studies. It seems to work by increasing the production of neurotransmitters which inhibit the sensations of pain. It also appears to play some role in controlling estrogens by helping their removal from the liver. The usual dose is in the range of 50-150 milligrams per day.
Essential Fatty Acids
Prostaglandins are involved in muscle contractions and menstrual pain and the fat that has the most prostaglandins are more beneficial. Omega-3 fatty acids seem to have the most anti-inflammatory properties rather than other fats. Some women adjust their fat balance by adding extra omega 3 rich oils such as flax oil to the diet. This counteracts the bad fats from meats and dairy products.
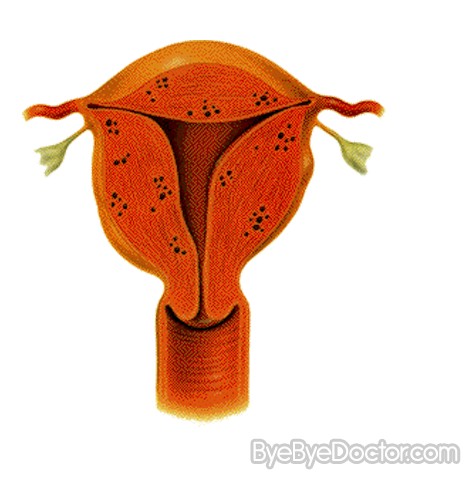
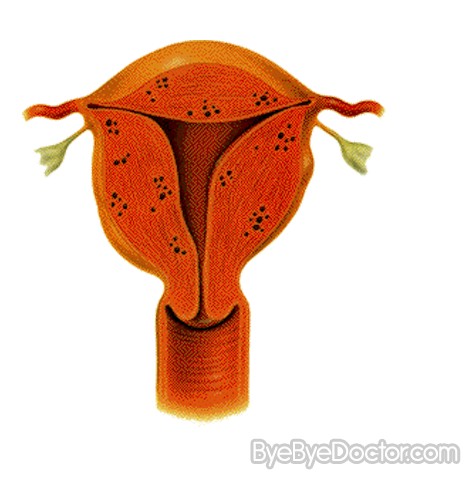
Adenomyosis Pictures

Thank you very much Ronnie, for this wonderful opportunity in sharing my wonderful experience.
ReplyDeleteI suffered from severe debilitating pelvic pain for over 9 years. It was thought that I had endometriosis but I had really adenomyosis. It was diagnosed after my hysterectomy. I also had multiple fibroids.
I have tried a lot of miracle supplements in the past, almost always experiencing some diverse side effect during the procedure. I am glad to say that I experienced no such effects during my stint with zomo product. Since I came across your product. Still, I did truly feel the impact of your wonderful herbal product. I felt a powerful spike in my energy levels during the first month of taken your herbal medicine, and a slight hike in sensitivity during the second month and beyond. I feel that this aspect of the treatment is most important, because a person may also gain a little insight into their overall health, now the pain is gone, also I started to change my diet, I eat more fish and fruits and vegetables. In March, I got another ultrasound and everything is OK now, hope it can help ladies in the same or similar situation. Here is his email: ronniemd70@gmail.com